What to take with intestinal infections with fever. Bacterial infections of the digestive system. Viral intestinal infections
Intestinal infection (or acute gastroenteritis) is a group of acute intestinal infectious diseases caused by the consumption of infected food products with characteristic symptoms of the stomach (lack of appetite, nausea, vomiting) and intestines ( varying degrees heaviness and discomfort in the abdomen).
In intestinal infections, microorganisms or toxins secreted by them cause poisoning.
More often, pathogens of intestinal infections give the name of the disease (for example, salmonellosis - salmonella, botulism - botulinum toxin, etc.). If the intestinal infection that caused the poisoning is not established, a diagnosis of "foodborne toxicosis" or "acute gastroenteritis" is made.
Types of intestinal infections transmitted with food
Food infectious poisoning are of different types.
- Acute poisoning caused by exotoxins (enterotoxins). Toxins produced by some microorganisms, violate the absorption in the intestine and cause increased intestinal production of electrolytes (salts of potassium, sodium, etc.) and water. Although normally these components should be absorbed by the intestines, and not stand out. Especially stormy secretions are caused by the cholera vibrio toxins.
- Acute poisoning caused by bacterial toxins that penetrate into the mucous membrane and. Toxins damage the intestinal wall, cause expressions, bleeding, secretion (secretion) of protein, water and electrolytes into the intestinal lumen. Such a process is observed in diseases caused by shigella (dysentery), salmonella and escherichia if it is (hemorrhagic colitis).
- Acute poisoning with little-known causes. These include diarrhea tourists.
- Acute infections of non-bacterial nature (). Poisoning can develop when ingested toxins contained in plants (for example, mushrooms) and food (fish, shellfish).
- Gastroenteritis resulting from product intolerance (hypolactasia), food allergies, heavy metal salts poisoning (arsenic, lead, mercury, cadmium) and side effects drugs.
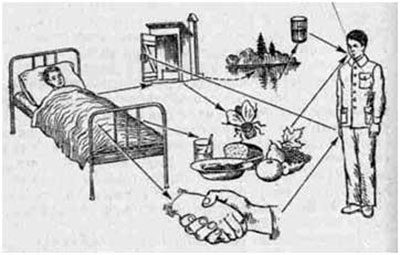
How does the infection occur?
Intestinal infections are not transmitted directly from a sick person to a healthy one. Their transfer is carried out by the fecal-oral route through food. In the case of single diseases, it is not always possible to establish the source of infection. In diseases of a group of people, the source of infection may be sick animals, humans or bacteria carriers.
Most often, intestinal infections are transmitted through meat, eggs, and convenience foods. The likelihood of infection when they enter the body is high (90% or more).
Symptoms
The characteristic symptoms of these diseases are:
- nausea,
- vomiting
- complete lack of appetite
- cramping abdominal pain,
- diarrhea, often with blood and mucus.
How does the disease develop?
Toxic poisoning infections begin acutely, suddenly. Sometimes from the outset, the disease is difficult.
Severe dehydration can develop as a result of constant vomiting and diarrhea. The sharp loss of water by the body can lead to a sharp drop in pressure and deterioration of the blood supply to the organs, which is very dangerous. In addition, oliguria (a sharp decrease in urine production) may develop.
If vomiting causes an excessive loss of fluid, then an increase in blood pH occurs due to the accumulation of alkali, a decrease in chlorine and potassium.
Abdominal distention is usually observed, in severe cases symptoms of peritoneal irritation appear. Gas-looped loops can be seen through the skin and felt to the touch.
With laboratory tests in patients with foodborne toxicoinfections in the acute period, there is a change in blood (leukocytosis), but there may be an increased content of leukocytes, the presence of red blood cells and protein in the urine.
Diagnostics
To establish the diagnosis of the patient's complaints are the primary, the definition of symptoms. It is important to find out if the disease is a single or affected group of people. The next important point to clarify the diagnosis are laboratory data.
Since the disease begins acutely with abdominal pain, it is first necessary to exclude acute diseases abdominal cavity.
Bacteriological examination of suspicious products, vomit and feces of the patient. The examination of the stool for bacteria should be carried out no later than 2 days after the onset of symptoms of poisoning.
At the same time, the isolation of one or another microorganism only from the material received from the patient does not give the right to consider it the causative agent of the disease, since many opportunistic bacteria that cause food toxicoinfections are often isolated from practically healthy individuals.
Evidence that one or another microorganism is the causative agent of this disease is the identity of the strains isolated from the patient and from the suspected products or from several simultaneously sick patients.
 Classification and nomenclature of causative agents of acute intestinal infections
Classification and nomenclature of causative agents of acute intestinal infections
In recent years, domestic and foreign researchers have obtained new data, expanding the previous ideas about etiology. acute intestinal infections (OCI) in children. The role of certain viral agents is convincingly substantiated and confirmed ( rotaviruses), enterotoxigenic Escherichia coli, Campylobacter, Yersinia, Clostridium, as well as the simplest - cryptosporidium and other microorganisms. Many of these microorganisms, however, have not yet been identified due to the lack of equipment in most domestic scientific and practical laboratories.
An essential feature of acute intestinal infections in children is their etiology. Diseases are caused by many different pathogens, among which pathogenic enterobacteria play an important role ( shigella, salmonella and enteropathogenic E. coli).
The presence of relatively widespread excretion of PFS in children and adults contributes to a significant seeding of the PFS environment, which, combined with a high resistance of PFS to action various factors the external environment can contribute to nosocomial infection of children.
Diseases caused by pathogenic enterobacteria
Shigellosis.
In the OCI series, a special place is occupied shigellosis, as this nosological form is more often than others ( with the exception of rotavirus infection) distributed by household contact among children and adults. The source of infection is a patient with an acute or erased form of dysentery. As known, children 1–2 years of age are most susceptible to shigellosis.
The group of dysenteric microbes, according to the new International Classification (1982), has 44 nomenclature units ( shigella serovars), included in 4 subgroups (A, B, C, D) of the Shigella species (S. dysenteriae - 12, S. flexneri - 13, S. boydii - 18, S. sonnei - 1).
Recently, the diseases caused by shigella Sonne and Flexner. Most often of shigella Flexnerin different years, serovars 2a, 6, and 1b were distinguished; from Shigella Sonne, biovars Ilq, He, la, Hid.
Endotoxins are part of the Shigella cell wall. . Shigi bacteria are capable of producing exotoxin, which has entero-, neuro-, and cytotoxic activity. At present, it has been proven that the bacteria Flexner and Sonne can synthesize similar toxins, but in smaller quantities. Shigella possess O-and K-antigens. O-antigen determines the serological specificity of Shigella, K antigens are shell structures.
Salmonella.
Salmonella, as well as Shigella, belong to the gram-negative rods of the family Enterobakteriaceae. Serologically for O- and H-antigens, these bacteria are differentiated into a number of serogroups, among which are the main A, B, C, D, E. In total, more than 2000 serovars are now known.however, most diseases in humans are due to few (10-15) salmonella serovars ( S. thyphim urium,S. haifa, S. infantis, S. panama, S. enteritidis, S. derby, S. anatum et al.). The intensity of the circulation of individual salmonella serovars can significantly increase in certain periods and in different territories.
The most susceptible to Salmonella children of the 1st year of life.
Salmonella infections in children of this age group are characterized by a variety of clinical manifestations. , and there are those that are extremely rare in older children, for example, sepsis, meningitis, meningoencephalitis, osteomyelitis, etc.. at the same time there is a high mortality in salmonellosis in newborns.
Both in our country and abroad, epidemic outbreaks in maternity hospitals, somatic and infectious hospitals, which are etiologically associated with the so-called "hospital" strains of Salmonella ( S. typhim urium, S. haifa, S. in fan tis, S. panama, etc..), polyresis to antibiotics. In children, the contact-household pathway of infection is of primary importance. Food route of infection is more common in salmonella in adults and older children.
Escherichiosis caused by enteropathogenic Escherichia coli (EPKP) of the genus Escherichia, which includes many representatives of normal microflora.
Currently, 168 O-groups are known in Escherichia coli (100 K- and 50 N-antigens). Strains capable of causing OKA belong to a relatively small number of serological groups.
OCI caused by ECPR, according to pathogenesis, clinic and epidemiological characteristics are heterogeneous.
Several infectious forms are known, each of which is caused by specific, inherent pathogens.
According to the modern classification of M. Levin (1987), colibacillosis is divided into 5 groups, respectively, the biopathogenetic properties of their pathogens. In the series of Escherichia that can cause diarrhea, there are:
1) EPKP - pathogens of colienteritis in children early agemainly 1st year.
2) Entero-invasive E. coli (EICP) - pathogens, dysenteria-like diseases in children (usually older than 1 year) and adults.
3) ETCS causative agents of choleroid diseases in children (mostly under 2 years old) and adults.
4) E nterohemorrhagic E. coli (EHEC) are the causative agents of OKA, occurring according to the type of hemocolitis and hemorrhagic uremic syndrome.
5) Enteric ("Adherent") E. coli (EAAC), which are identified only in Hep-2 tissue culture (gray groups not yet defined). EAACs are a fairly common cause of diarrhea among tourists in Mexico, their role in other types of diarrhea is not yet clear.
EPKP in 15-20% of cases are the cause of diarrhea in children. The frequency of EECP detection usually does not exceed 2-4%. The significance of ECDPs as OCI pathogens varies from 2-7 to 20-30% of the number of registered OKI. EGPK 0 1b7: H, described relatively recently, has not yet been identified in our country (there is no corresponding agglutination serum). These strains contain the plasmid 60 MD and produce two types of Shig-like toxins (Verotoxin-1 and -2). In Canada, sporadic and group diseases that are etiologically associated with this pathogen are registered.
The important role of EHEC in the etiology of hemocolitis and hemorrhagic uremic syndrome in young children in Czechoslovakia was noted.
It is shown that one of the most important features colienteritis is its ability to nosocomial proliferation. Most of the nosocomial diseases were caused by EPKP 4 serological groups (O20, Osh, 0 I9, 0 142), which, unlike those of other serogroups, are resistant to the maximum number of antibiotics.
Etiological structure of OKA reflected only in selected publications of domestic authors. According to these researchers, in children aged 0–2 years in the structure of OKA, shigellosis, salmonella and escherichiosis accounted for 1, 9–13.3, 13–26.5 and 4.7–38%, respectively, in older children, 10.8–59, 2.7–10 and 10.3–11 ,five% .
Intestinal yersiniosis.
Causative agent of intestinal yersiniosis - Yersinia enterocolitika (Y.e.) - gram negative family Enterobacteriaceae. According to the scheme W auters (1971), in Y.e. 30 O-groups were determined for O-antigen. The overwhelming majority of strains isolated from people with intestinal yersiniosis disease belong to 0 3 and 0 9 serovars, less often to 0 8, 0 5, 0 27 and O6.O30 serovars.
Diseases, according to the literature, are characterized by extreme polymorphism. However, most often, especially in children, occurs intestinal form of yersiniosis with gastroenteritis or enterocolitis syndrome. Foreign researchers indicate that approximately 5% of all sporadic diarrhea are etiologically associated with Yersinia.
In the domestic literature, the works devoted to the study of this nosological form in children are few.
Diseases caused by so-called opportunistic enterobacteria.
In recent years, there are more and more reports about the role of EPE in etiology. OKI in children. Despite the significant number of works devoted to this problem, there is no single point of view on the role of PEI in the occurrence of diarrhea.
According to N.M. Gracheva, verification of the diagnosis of sporadic cases of OCI caused by UEI is still difficult and not always convincing. In this regard, many researchers limit themselves to the quantitative and qualitative characteristics of the intestinal microflora in patients, without touching upon the verification of the diagnosis.
It is noted that these OCI mainly suffer from young children with an unfavorable premorbid background, who are on artificial or early mixed feeding. The frequency of isolating Proteus in patients with OCI in children ranges from 11.2 to 39.4%, Klebsiella is from 11 to 17%, reaching 19-52% in the group of children of the first year of life. In OCI patients, Proteus and Klebsiella of certain serological varieties were most often found.
There are reports of domestic and foreign authors about the etiological role of not only klebsiellbut others citrapositive enterobacteria (enterobacter, citrobacter and others) for acute intestinal and intrahospital infections.
OCI, etiologically associated with IPE (Proteus, Klebsiella, Enterobacter, Citrobacter, etc.), in recent years, they have been quite widely diagnosed by practical laboratories, and, as a rule, on the basis of studying the enzymatic properties of the isolated cultures.
The diagnosis is considered justified with a massive amount of IPE (105 or more in 1 g of faeces) in the first days of the disease and serological confirmation with an autostrain.
Meanwhile, the allocation of IPE from feces is often observed in practically healthy individuals. Very often there is a secondary detection of these antigens due to dysbacteriosis, which develops under the influence of the main etiological factor OKA or (as is often observed in children), in case of illness of other organs and systems. In dysentery and salmonellosis, as a rule, accompanied by the development of intestinal dysbiosis, in 41.9 and 45.7% of cases, respectively, EPE were allocated in large quantities (105 and more in 1 g of material), including 2 -3 types of EPE and more 17.9 and 18.6% of patients.
It is known that the so-called IPE has a complex antigenic structure. Thus, in bacteria of the genus Citrobacter, 42 O-groups and 90 N-antigens are found, in the E. Cloaceae species - 53 O-antigens, in the K. Pneumea species - 12 O- and 82 K-antigens, etc.
For the scientific substantiation of the etiological role of OCI representatives of the genera klebsiella, citrobacter, Proteus et al. it is important to be able to subject these microorganisms to serological typing.
However, this method of research is not yet sufficiently accessible. In the case of substantiation of the etiological role of IPE, isolated from patients with acute intestinal infections, even from the source of an epidemic outbreak with a single source of infection, it is necessary to establish not only their cultural-enzymatic, but also antigenic unity.
Staphylococcal infection.
According to some researchers, one of the frequent forms of OCI is staphylococcal infection, the causative agent of which is Staphylococcus aureus.
Diseases in children are more commonly caused by Staphylococcus aureus. . The pathogenicity of staphylococcus is determined by its biological properties: the ability to release toxins (enterotoxin, etc.), enzymes (coagullase, lecitovitellase) and other biologically active substances.
OCI of staphylococcal nature can develop as a result of primary infection of the intestine, and during its secondary penetration into the intestine from parenchymal foci of inflammation ( pneumonia, otitis), with generalized infection ( sepsis) or as a result of intestinal dysbiosis. Susceptibility to this infection is highest in newborns and children in the first year of life.
Diagnosis of OCI of staphylococcal nature should be very responsible, since in practice there are both overdiagnosis and underdiagnosis, as evidenced by the large difference in the frequency of detection of staphylococcal bowel lesions among children hospitalized in the diagnostic departments. If we take into account that in 1/3 cases staphylococcal enteritis and enterocolitis turn out to be diseases of mixed etiology, then it becomes clear how important it is to correctly resolve the issue of the true meaning of staphylococcus in the development of intestinal disease.
In recent years, there has been a significant increase in the frequency of mixed bacterial and bacterial-viral infections, especially in young children. The most important associates are noted. pathogenic staphylococcusEPKP salmonella, as well as the IPE ( klebsiella Proteus and so on.) and rotaviruses. It is indicated that a mixed intestinal infection is observed more often in debilitated children who were more often on artificial feeding.
They proceed, as a rule, are heavier and longer than monoinfection.
Anaerobic infections of bacterial troll
Campylobacteriosis.
Special attention of specialists in recent years has attracted campylobacteriosis, which is due to its extremely wide spread abroad, the intensive circulation of the pathogen among people and various animals, high morbidity rates and great socio-economic damage from this infection.
Originally campylobacter were attributed to the Vibrionaceae family, but their morphological characteristics differed significantly. In 1963, a new genus, Campylobacter, of the family Spoirallaceae was created.
He included C. fetus and related microorganisms. Although the genus Campylobacter includes more than 10 species, found both in animals and in humans, but the greatest value as causative agents of acute diarrhea in humans have C. jejuni, S. coli, C. laridis, C. fetus. In patients with reduced immunity, including those with HIV infection, enteritis and enterocolitis can cause S. cinaedi, S. fennelliae and campylobacter-like organisms . C. Fetus spp. fetus most often affects patients who are weakened by intercurrent diseases and causes a hematogenous disseminated infection with the formation of purulent septic foci. Overwhelmingly campylobacterios, both in children and adults due S. jejuni.
Campylobacter - thin movable Gram-negative, non-sporiferous curved rods, comma-shaped or S-shaped, of a length of 0.5 to 0.8 microns, thickness of 0.2-0.0 microns. Characteristic helical movements are due to the presence of one or two polar flagella with a length of up to 15 microns. Polymorphism is common among these cells. Modified forms are represented by curved or spiraling microorganisms that are variable in length and thickness. In old cultures, spherical and coccoid cells predominate.
Campylobacter microaerophiles.
The strains of C. jejuni grow better at a temperature of 42 ° C and the following gas composition: 0 2-5%, C02- 10%, N2- 85%. C. fetus can grow in anaerobic conditions.
To isolate campylobacter from feces, selective media can be used that inhibit the growth of other enteropathogenic bacteria.
Usually, nutrient media enriched with blood (5-10% of sheep, rabbit or horse blood) and a mixture of antibiotics are used for these purposes. There are several commercial selective nutrient media: medium Skirrowwednesday Butzlerwednesday With Atru-Varwednesday Preston and others. Enrichment media have been developed.
S. jejuni form colonies of two types. Some of them are wet, slimy, flat, “sprawling”, with uneven edges. Often, colonies are very flat and look like condensate of water vapor. Others - convex, shiny, with a diameter of 1-2 mm.
Campylobacter contain thermostable and thermolabile antigens. O and H antigens studied C. fetus. The most important surface antigens are lipopolysaccharides and the acid soluble protein fraction. All serotypes of Campylobacter have a common protein antigen contained only in flagella.
Clostridioza.
Etiological role Clostridium difficile and their toxins proved by a number of foreign researchers in the 70s with pseudomembranous colitis resulting from antibiotic therapy. In recent years, these bacteria are increasingly seen as OCI pathogens.
Indicates the possibility of nosocomial infection.
Cl. difficile - large mobile gram-positive rods, which are strict anaerobes.
They form oval sub-terminal spores and produce two types of thermolabile toxin - enterotoxin A and cytotoxin B. According to foreign researchers, the frequency of detection of this pathogen in patients with acute intestinal infections ranges from 11.9 to 59% (in newborns). Diarrhea caused by C1. difficile, are described in Sweden, Canada, USA and other countries. A number of Moscow researchers have attempted to develop methodological approaches for the laboratory diagnosis of intestinal clostridiosis caused by Cl. difficile. Laboratory diagnosis of diarrhea caused by clostridia of this species is based on detection in faeces. Cl. difficile and their identification, as well as on the determination of toxins in the test on cell cultures and in experiments on the infection of white mice.
Aeromonal infection
Aeromonads belong to the family Aeromonadaceae. Rod Aeromonas includes more than 5 species. Pathogenic for people consider the view A. hydrophila, many strains of which produce thermostable enterotoxin and cytotoxin. Entero-oxygenated aeromonad cultures isolated with OCI usually have the ability to produce hemolysin and hemagglutinin. These cultures produce oxidase and give a positive Voges-Proskauer reaction. Both sporadic cases of disease and outbreaks are described. Seasonal growth of diseases caused by aeromonas is observed in summer. At the same time, they are often isolated from surface waters, which gives reason to consider water as one of the factors of transmission.
Airborne diseasestend to flow easily. The characteristic symptoms are watery diarrhea, vomiting, low-grade fever, and abdominal pain. Cases and more are described. heavy current diseases.
Plesiomonasal infection
The causative agent of this disease, Plesiomonas shygelloides, belongs to the family of Vibrionaceae. Plesiomonad- Rod-shaped bacteria, facultative anaerobes. In species P . shygelloides30 O-antigens and 17 variants of H-antigens were detected. Cultures of this species produce both thermolabile and thermostable enterotoxins. They possess oxidase and catalase activity, they ferment glucose with the formation of acid, and they give a negative reaction of Fores-Proskauer.
Abroad plesiomonad isolated from patients with enteritis and healthy people, from fresh and sea water, as well as from cats, dogs and other animals.
Especially often these diseases are recorded in tropical and subtropical countries. In Europe (France, Great Britain, Czechoslovakia, and others), isolated cases of dysentery-like diseases caused by plesiomonads are described. Plesiomonas infection it is more common in children than in adults, but the youngest children are least affected by this infection.
Rotavirus gastroenteritis
Rotavirus infection - A widespread and ubiquitous disease, affecting mainly young children.
Rotaviruses cause acute diarrhea in 20-40% of sick children. Described outbreaks of rotavirus infection, including nosocomial. The characteristic of the clinical manifestations of the disease. The most common clinical signs of rotavirus infection in children have been shown to be diarrheal syndrome, fever and vomiting - 98.9, 82 and 75%, respectively.
Rotaviruses are genus of family Reoviridae, which combines a large number of similar in morphology and antigenic structure of viruses that cause gastroenteritis in humans, mammals and birds. The causative agents of rotavirus gastroenteritis are divided into two subgroups (I and II), which include viruses of 4 serotypes (1, 2, 3, 4). Some rotaviruses isolated from animals have common antigens with human rotavirus (the Nebraska calf virus belongs to the 1st subgroup, the monkey SA11 virus - to serotype 3 of the same subgroup). This allows you to use these viruses, well cultivated in vitro, for the formulation of immunological tests for laboratory diagnosis of viral gastroenteritis.
For detection of rotaviruses and antigens in feces, they use electron microscopy, enzyme-linked immunosorbent assay, polyacrylamide gel electrophoresis, latex agglutination with Rolatex test system (Finland), and the method of counter-immunoelectrophoresis with highly active rabbit serum, immuno-immunoassay. rotavirus diarrhea calves (strain of Nebraska), proposed by Yu. N. Mastyukova and auth. (1985) and others. Unfortunately, to date, in most cases, these diseases remain etiologically undeciphered due to the lack of an established system of laboratory diagnosis of rotavirus infection. Abroad for the detection of rotaviruses use commercial test systems "Rotazime" (USA), "Enzygnost" (Germany), "Dakopatts" (Denmark). In our country, developed a set of "Rotapast-1".
Diseases caused by protozoa
Cryptosporidiosis.
The causative agent of cryptosporidiosis are coccidia of the genus Cryptosporidium tyzzer (family Cryptosporididae leger). They have long been considered non-pathogenic protozoa. The first cases of cryptosporidiosis were recorded in the early 70s.
In recent years, extensive material has been accumulated abroad on the clinical and epidemiological features of cryptosporidiosis, the diagnosis and treatment of this invasion. The frequency of isolation of pathogens of cryptosporidiosis in young children in different countries varies from 0, 7 -1, 3% (in Spain, Germany, China) to 18.4-21% (in South Africa, Nigeria).
There were reports of the identification of patients with cryptosporidiosis in the Russian Federation. All patients had fluid, watery stools, and a number of them had nausea, vomiting, fever, and abdominal pain.
The list of OCI pathogens in children can be extended at the expense of other bacterial and viral agents. In the literature, in particular, there are reports of a possible role in the etiology of enterobacteria diarrhea Edwardsiella tarda, Serratia marcescens, as well as caliciviruses and other microorganisms. More detailed information about the OCI pathogens considered in this material can be obtained from numerous reviews and monographs published in recent years by domestic and foreign authors.
The analysis of the literature data indicates the etiology of OCI in children. The causative agents of these diseases, along with traditional pathogenic enterobacteria, can be many other bacterial and viral agents ( yersinia, Campylobacter, Rotavirus, Clostridium, Aerial and Plesiomonad, etc..) and the simplest ( cryptosporidia). Some are suspected of causing OCI pathogens in weakened young children klebsiella, Proteus, Citrobacter, Enterobacter, etc.).
Extensive identification and identification of the above microorganisms is possible only with the continuous improvement of laboratory diagnostics of AEI. To this end, research should be continued (at a higher methodological level with the study of the antigenic structure of the isolated cultures) to clarify the etiological role of the little-studied pathogens of the OKA, including the TEA. It is also necessary to accelerate the study of the DNA hybridization method currently widely used abroad, which allows not only to detect various bacteria and viruses in pathological material, but also to successfully use DNA probes to identify OKI pathogens and determine their toxins. The ultimate goal of these studies should be the development of simplified DNA probes for practical use.
If you find an error, please highlight a piece of text and click Ctrl + Enter.
Types of intestinal infections are completely different, but all of them can not only undermine health and cause long-term discomfort, but also lead to far more serious consequences if they are not cured in time. One of these infections can be picked up at any time of the year (especially in the summer when they are most active), and every year doctors regret to say that there are regular outbreaks of diseases caused by E. coli or rotavirus infection. And there are a lot of other pathogens: Salmonella, Escherichia, Staphylococcus, Enterovirus, Shigella, Amoeba, Fungi and many others. Of course, the most common symptoms of these diseases are abdominal pain, nausea and diarrhea, however, a detailed classification of all possible intestinal infections will be needed in order to understand their differences and subsequent treatment methods.
Viral intestinal infections
The first thing to be aware of is that intestinal infections can be viral and bacterial, with the first of them being further divided into three categories: rotavirus, enterovirus and adenovirus types.
In all cases, the main routes of infection are noncompliance with simple rules of sanitation and hygiene (through dirty food, hands or objects), as well as penetration of the pathogen into the body through an airborne droplet.
If we talk about enteroviruses, then this disease occurs with a number of acute symptoms that can be completely different (which makes it difficult to diagnose):
- muscle pain;
- fever;
- convulsions;
- drowsiness;
- tearfulness of the eyes;
- tachycardia;
- weakness;
- heartache;
- runny nose and sore throat;
- diarrhea.
Such a symptom as high temperature remains unchanged, while other symptoms depend on the type of enterovirus, which can affect both muscles and the nervous system, skin, cardiovascular system.
In turn, adenovirus infection is not very common and affects mainly the mucous membranes of the eyes and nose, but if the pathogen enters the small intestine, it can provoke vomiting, diarrhea and loss of appetite (although all symptoms usually disappear within a couple of days).
 Finally, the most common viral type of intestinal infections is rotavirus, which is also called gastric or intestinal flu. The incubation period can last from one to five days, after which the disease enters the active phase, and during this period the person must be isolated from others to prevent the spread of the virus. Both adults and children are affected, who suffer it somewhat harder. Symptoms are generally similar to enterovirus infections and consist of high fever (up to 39 degrees), diarrhea, vomiting, acute pain in the stomach, runny nose and throat inflammation. Again, the cause is often caused by unsanitary conditions - contaminated food or hands, and almost always a person “gets acquainted” with this ailment even in kindergarten or a school where rotavirus outbreaks are common. However, over time, the body begins to more effectively fight the infection, producing immunity to it, so that each subsequent case is more easily tolerated than the past.
Finally, the most common viral type of intestinal infections is rotavirus, which is also called gastric or intestinal flu. The incubation period can last from one to five days, after which the disease enters the active phase, and during this period the person must be isolated from others to prevent the spread of the virus. Both adults and children are affected, who suffer it somewhat harder. Symptoms are generally similar to enterovirus infections and consist of high fever (up to 39 degrees), diarrhea, vomiting, acute pain in the stomach, runny nose and throat inflammation. Again, the cause is often caused by unsanitary conditions - contaminated food or hands, and almost always a person “gets acquainted” with this ailment even in kindergarten or a school where rotavirus outbreaks are common. However, over time, the body begins to more effectively fight the infection, producing immunity to it, so that each subsequent case is more easily tolerated than the past.
There is a strong resistance of this type of pathogen to cold temperatures, making the disease is seasonal and most dangerous in the winter.
It must be remembered that the disease is transmitted by airborne droplets, so an infected person can become the culprit of infection and other people if he is not provided with quarantine.
Unfortunately, there are no drugs for rotaviruses, so the patient is prescribed drugs that directly suppress the symptoms of the disease:
- antipyretic;
- knitting;
- lactic;
- adsorbing.
Rotavirus intestinal infection, as a rule, does not lead to complications if therapy was started on time, but a couple of important points should be remembered: firstly, if vomiting or diarrhea are frequent and prolonged, the patient must be provided with a constant drink to replenish the water-salt balance and prevent dehydration. Secondly, rotaviruses do not tolerate well elevated temperature body, but because doctors do not recommend lowering it below 38 degrees - this will contribute to a more rapid death of pathogens. Finally, during this period, it is necessary to stick to a diet, and boiled rice or chicken broth will be the most preferable. With a favorable course of events, the disease will recede in five to seven days.
Bacterial intestinal infections
The classification of bacterial infections of the intestine has many types of bacteria, the main diseases are:
- staphylococcal infection;
- colibacillosis;
- klebsiella;
- yersiniosis;
- protozoal infections;
- fungal infections.
 Salmonella infection is a fairly widespread disease, active throughout the year, while Salmonella bacteria are very tenacious, which is an additional danger. The fact is that they die at a temperature of at least 70 degrees, and then after 10 minutes, and therefore they can survive inside a thick piece of meat with insufficient heat treatment - boiling, salting or smoking. While active, the bacteria remain for several months, affecting people, animals and birds. Actually, it is poultry or animal meat that is the most common method of infection with salmonella, however, like some dairy products (in addition to contacts with carriers of the virus). It is most difficult for children to suffer from this intestinal infection, and its classification is as follows:
Salmonella infection is a fairly widespread disease, active throughout the year, while Salmonella bacteria are very tenacious, which is an additional danger. The fact is that they die at a temperature of at least 70 degrees, and then after 10 minutes, and therefore they can survive inside a thick piece of meat with insufficient heat treatment - boiling, salting or smoking. While active, the bacteria remain for several months, affecting people, animals and birds. Actually, it is poultry or animal meat that is the most common method of infection with salmonella, however, like some dairy products (in addition to contacts with carriers of the virus). It is most difficult for children to suffer from this intestinal infection, and its classification is as follows:
- localized;
- generalized;
- excretion of bacteria.
Localized is considered the most common and manifests itself already on the first day of infection through fever, fever, abdominal pain, diarrhea and vomiting. Far more dangerous are possible complicationsconcomitant salmonellosis, to which doctors include cerebral edema, cardiac and renal failure, disorders in the adrenal glands.
Staphylococcus bacterium is considered conditionally pathogenic, since in the normal state of the intestinal microflora it does not pose a threat, but it is activated with reduced immunity or after antibiotic therapy.
Against the background of such situations, staphylococcal intestinal infection develops rather slowly, and the first symptoms are a runny nose and sore throat, as well as a not very high temperature - because of this, the onset of the disease is sometimes confused with the common cold.
The rest of the clinical picture varies from case to case, resembling a typical food poisoning. The symptoms described are as follows:
- abdominal pain;
- vomiting;
- bloody;
- skin rashes;
- general weakness.
As you know, staphylococcus bacteria multiply rapidly in environments with temperatures above 20 degrees, and often food such as eggs, meat, fish, creams and dairy products, cakes, salads and others can be the cause of infection. It remains to add that although staphylococcus is currently studied in as much detail as possible, it is difficult to treat the infection it causes due to its mutational abilities and resistance to antibiotics.
 Another bacterial intestinal infection is the long-known typhoid fever, a disease caused by one of the varieties of salmonella, and in some cases can cause death.
The cause of the disease, of course, is the same violation of personal hygiene, as well as infection from the carrier of the infection. Sometimes it can be caused by contact with feces or urine infected, sometimes by dirty water or food. Insects like flies are considered another carrier. The incubation period takes up to two weeks, after which a person's temperature rises, his throat and joints start to ache. Following this, abdominal pain and recurrent nasal bleeding appear (pain is possible during urination). Diagnosing typhoid fever is sometimes quite difficult, as it can cause symptoms similar to diseases of the urogenital system or pneumonia.
Another bacterial intestinal infection is the long-known typhoid fever, a disease caused by one of the varieties of salmonella, and in some cases can cause death.
The cause of the disease, of course, is the same violation of personal hygiene, as well as infection from the carrier of the infection. Sometimes it can be caused by contact with feces or urine infected, sometimes by dirty water or food. Insects like flies are considered another carrier. The incubation period takes up to two weeks, after which a person's temperature rises, his throat and joints start to ache. Following this, abdominal pain and recurrent nasal bleeding appear (pain is possible during urination). Diagnosing typhoid fever is sometimes quite difficult, as it can cause symptoms similar to diseases of the urogenital system or pneumonia.
The greatest danger is represented by complications, manifested in the form of incoherent delirium, stupor or even coma, because of which the subsequent recovery process may take years (although the overall forecast is pessimistic). In addition, when inadequate treatment the infection can provoke bleeding in the intestine until it is perforated, which leads to peritonitis. If the pathogen enters the bloodstream, the following organs may be affected:
- gallbladder;
- liver;
- brain membrane;
- genitals;
- heart valves;
- kidneys;
- bone marrow.
At risk are small children and old people, as well as patients with weak immunity, which significantly increases the statistics of mortality in typhoid fever. It should be added that after complete recovery, 10% of those who have been ill will eventually be diagnosed with a recurrent disease.
Intestinal coli infection is otherwise called colibacillosis, as it is caused by the bacteria of the same name - Escherichia. This is another infection that affects the intestines and causes symptoms such as vomiting and diarrhea, but in rare situations, the biliary tract, the urinary system and the lungs can suffer. Most often, small children suffer from it, and premature babies with weak immunity are most at risk. Actually, children are one of the most common causes infection with coli-infection of surrounding people, and the classical method of transmission of the pathogen is the fecal-oral route: contact with people, clothing, objects, products to which Escherichia are transferred.
 The intestinal infection caused by the Klebsiella bacterium is acute, as it is accompanied by abdominal pain, vomiting, diarrhea and high fever. In addition to young children and old people, it most often affects people with immunity weakened after the operation, as well as patients with diabetes, cancer, and blood diseases. Alcoholism can become another contributing factor, and Klebsiella can be treated with probiotics and bacteriophages.
The intestinal infection caused by the Klebsiella bacterium is acute, as it is accompanied by abdominal pain, vomiting, diarrhea and high fever. In addition to young children and old people, it most often affects people with immunity weakened after the operation, as well as patients with diabetes, cancer, and blood diseases. Alcoholism can become another contributing factor, and Klebsiella can be treated with probiotics and bacteriophages.
Another pathogenic bacterium is coccobacillus, which causes an intestinal infection called yersiniosis, most often in infants, young people and adult men. Usually its carriers are animals like rodents or livestock, and it can remain active even under adverse environmental conditions. Symptoms include:
- diarrhea;
- pain in the abdomen;
- fever;
- in rare cases, blood poisoning.
With timely treatment and strong immunity, Yersiniosis passes within a few days, although this treatment is purely symptomatic in view of the unproved effectiveness of antibiotics. However, in more severe cases, antimicrobial therapy can be prescribed using drugs such as fluoroquinolone, cephalosporin, biseptol and aminoglycosides.
Protozoal intestinal infections comprise dozens of species, and the risk of diseases caused by these protozoa microorganisms is rather high among the population, according to competent specialists. First of all, various organs and tissues such as the intestines, lungs, circulatory system, nervous system and others suffer. In addition to the standard pathway (as well as through sexual contact), insects that bite a person often act as carriers. The list of the most common protozoal infections is as follows:
- trypanosomiasis;
- malaria;
- amebiasis;
- giardiasis;
- infusorial dysentery;
- leishmaniasis;
- toxoplasmosis;
- trichomoniasis.
The most famous intestinal fungal infection is candidiasis, excessively activated in the intestine due to weak immunity or taking antibiotics. wide spectrum, corticosteroids or laxatives. All of these factors disrupt the normal microbiocenosis of the intestine, due to which the body loses its ability to effectively fight pathogenic fungal pathogens. It is necessary to treat candidiasis with locally active medications under a diet that excludes the use of alcohol, as well as sugary, fatty, and fried foods. It is important to add that in women, candidiasis that develops in the intestines can lead to vaginal candidiasis (thrush).
Important!
HOW TO REDUCE THE RISK OF CANCER CANCER?
Time limit: 0
Navigation (mission numbers only)
0 out of 9 tasks completed
Information
PASS FREE TEST! Thanks to the detailed answers to all the questions at the end of the test, you will be able to REDUCE the probability of the disease!
You have already passed the test before. You cannot start it again.
Test loading ...
You must login or register to start a test.
You must complete the following tests to begin this:
results
Time is over
1. Can cancer be prevented?
The occurrence of a disease like cancer depends on many factors. Ensure full safety can not no one. But significantly reduce the chances of malignant tumor everyone can.
2. How does smoking affect cancer?
Absolutely, absolutely forbid smoking. This truth is already tired of all. But quitting smoking reduces the risk of developing all types of cancer. Smoking is associated with 30% of deaths from oncological diseases. In Russia, lung tumors kill more people than tumors of all other organs.
Excluding tobacco from your life is the best prevention. Even if smoking is not a pack a day, but only half, the risk of lung cancer is already reduced by 27%, according to the American Medical Association.
3. Does overweight influence cancer development?
Look at the scales more often! Extra pounds will affect not only the waist. The American Cancer Research Institute has found that obesity provokes the development of tumors of the esophagus, kidneys and gallbladder. The fact is that adipose tissue serves not only to save energy reserves, it also has a secretory function: fat produces proteins that affect the development of a chronic inflammatory process in the body. And cancer just appear on the background of inflammation. In Russia, 26% of all cases of cancer WHO is associated with obesity.
4. Will sports contribute to cancer risk reduction?
Give workouts at least half an hour a week. Sport is on the same level with proper nutrition when it comes to oncology prevention. In the United States, one third of all deaths are attributed to the fact that patients did not follow any diet and did not pay attention to physical education. The American Cancer Society recommends training for 150 minutes a week at a moderate pace, or two times less, but more active. However, a study published in the journal Nutrition and Cancer in 2010, proves that even 30 minutes is enough to reduce the risk of breast cancer (which affects every eighth woman in the world) by 35%.
5. How does alcohol affect cancer cells?
Less alcohol! Alcohol is blamed for the occurrence of tumors of the oral cavity, larynx, liver, rectum and milk glands. Ethyl alcohol breaks down in the body to acetic aldehyde, which is then transformed into acetic acid by the action of enzymes. Acetaldehyde is the strongest carcinogen. Alcohol is especially harmful to women, since it stimulates the production of estrogen - hormones that affect the growth of breast tissue. Excess estrogen leads to the formation of breast tumors, which means that every extra sip of alcohol increases the risk of getting sick.
6. What cabbage helps fight cancer?
Like broccoli cabbage. Vegetables are not only included in a healthy diet, they also help fight cancer. In particular, therefore, recommendations on healthy nutrition contain a rule: vegetables and fruits should make up half of the daily diet. Especially useful are cruciferous vegetables, which contain glucosinolates - substances that, during processing, acquire anti-cancer properties. These vegetables include cabbage: regular white cabbage, Brussels sprouts and broccoli.
7. Which body cancer is affected by red meat?
The more you eat vegetables, the less you put in a plate of red meat. Studies have confirmed that people who eat more than 500 grams of red meat a week have a higher risk of getting rectal cancer.
8. What remedies are suggested to protect against skin cancer?
Stock up on sunscreen! Women aged 18–36 years are particularly susceptible to melanoma, the most dangerous form of skin cancer. In Russia, in just 10 years, the incidence of melanoma has increased by 26%, world statistics show an even greater increase. This is blamed on the equipment for artificial tanning, and the sun's rays. Danger can be minimized with a simple tube of sunscreen. A 2010 study by the Journal of Clinical Oncology confirmed that people who regularly apply a special cream suffer from melanoma two times less than those who neglect such cosmetics.
The cream should be chosen with the SPF 15 protection factor, applied even in winter and even in cloudy weather (the procedure should become the same habit as brushing your teeth), and not be exposed to sunlight from 10 to 16 hours.
9. What do you think, do stresses affect the development of cancer?
By itself, the stress of cancer does not cause, but it weakens the entire body and creates the conditions for the development of this disease. Studies have shown that constant anxiety alters the activity of immune cells responsible for the inclusion of the “hit and run” mechanism. As a result, a large amount of cortisol, monocytes and neutrophils, which are responsible for inflammatory processes, constantly circulate in the blood. And as already mentioned, chronic inflammatory processes can lead to the formation of cancer cells.
THANK YOU FOR YOUR TIME! IF THE INFORMATION WAS REQUIRED, YOU CAN LEAVE FEEDBACK IN THE COMMENTS AT THE END OF THE ARTICLE! WE WILL BE GRATEFUL!
- With the answer
- With a mark of viewing
Task 2 of 9
How does smoking affect cancer?
Task 3 of 9
Does overweight affect cancer development?
Task 4 of 9
Do physical exercises reduce cancer risk?
Task 5 of 9
Task 1 of 9
Is it possible to prevent cancer?
A very common disease is intestinal infection, which implies a violation of activity gastrointestinal tract. According to statistics, the first place is occupied by a group of acute respiratory diseasesand the second most common are
It is worth noting that children are at risk, since their bodies are not yet ready to fight such a serious infection. The proportion of childhood deaths due to the development of the tract is very high. To prevent such consequences, first of all, it is necessary to observe the elementary. These include compulsory hand washing and all products, especially fresh vegetables and fruits. It is worth paying attention to the water that the child consumes: it must be filtered. Killing bacteria is also possible by boiling. Since childhood, it is necessary to instill simple rules for children, for example, that after the toilet you should wash your hands without fail.
Such precautions can protect a person from serious consequences, because an intestinal infection spreads quickly in the body. The incubation period of any bowel disease is from 12 hours to 2 days, during which time the virus manages to get comfortable in the microflora and begin to act.
Intestinal infection: species
- Cholera
- Food poisoning
- Dysentery
- Staphylococcus
- Enterovirus
- Salmonellosis
- Typhoid fever
After certain types of diseases, immunity is produced, that is, the body's ability to produce antibodies and prevent the development of infection. These include staphylococcus, cholera. Immune protection can be lifelong or for a period of time.
Intestinal infection: signs
At the first stage of the disease, the patient feels a general weakness of the body, while constantly twisting the abdomen. Gradually his condition worsens, the main symptoms begin to appear. Pursues a constant feeling of nausea, which is accompanied. Most often there is severe diarrhea, on the basis of which there is a sharp increase in temperature. Often causes painful sensations in the area of the stomach. Subsequently, there is a decrease in pressure, which causes loss of consciousness when adopting a vertical position. The patient becomes cold, tormented by a severe chill.
The greatest danger to human life are symptomatic manifestations of the disease. For example, with severe diarrhea, there is a sharp loss of fluid, that is, dehydration. Then a patient who is engaged in self-treatment (that is, without the help of a doctor) can die within a few days.
As a rule, the intestinal infection is treated in a hospital, in order to ensure the patient is constantly monitored by qualified personnel. First of all, droppers are prescribed to a person with dehydration, and abundant drinking is recommended. Depending on the type of disease and its severity drug treatment. If a severe infection is found that cannot be overcome by the body itself, antibiotics are prescribed. In case of usual poisoning, sorbents are assigned to
All attempts to recover on their own or with the help of information found in the global network can be fatal, because there are cases when the clock is spent on time. If you go to a specialist in time, the disease will be much easier. A qualified treatment will give a quick result and, as a result, full recovery and return to the previous life.
Intestinal infection is a concept that combines many different diseases. The cause of their appearance are viruses and bacteria, as well as toxins, which are produced in the course of their life. Almost every person faces this problem at least once in their life. In order to avoid such unpleasant situations, it is necessary to understand the features of the disease, the features of infection and the emerging symptoms.
Intestinal infection combines about 30 diseases.. They develop under the action of pathogenic microorganisms. Damage occurs first digestive system.
Regardless of the type of microorganism that provoked the development of the disease, intestinal infections begin acutely and have common symptoms. There are signs of general intoxication of the body, as well as special manifestations, which can identify the causative agent of the problem.
Intestinal infections affect people of all ages, including infants. There are several different ways infection. At risk are children, old people, people suffering chronic diseases or alcoholism.
The main causes of the disease
The cause of the development of the disease becomes ingestion of pathogenic microorganisms.. This can occur in several ways: 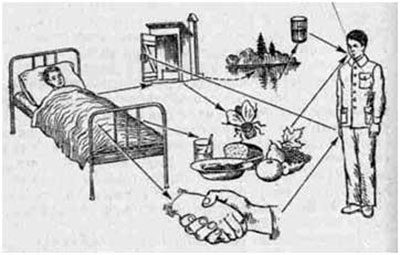
- Contact with dishes or food of infected rodent or insect feces.
- Violation of food storage standards. It is impossible to store raw meat or fish and fruit on the same shelf of the refrigerator, which before consumption will not undergo heat treatment.
- Insufficient heat treatment of products. Most pathogenic microflora dies when heated above 70 degrees.
- Violation of temperature storage of food. Especially it concerns confectionery and sausages, milk-containing products, as well as cooked dishes. Under the condition of room temperature, microorganisms enter the phase of active reproduction.
- The use of low-quality products that are infected with microorganisms.
- Consumption of contaminated water.
In order to prevent infection, it is necessary to closely monitor the quality of drinking water and food, as well as observe the rules of storage and cooking.
If you are not sure about the safety of food, it is better to throw it away. Even the slightest signs of damage indicate that the entire product is infected and its use is dangerous to health.
What causes the disease
Penetrating into the human body, bacteria have a negative effect on the mucous surfaces of the intestines and stomach. Starts inflammatory process. Its localization leads to the following comorbidities: 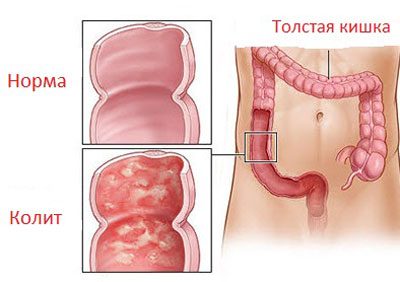
- Enteritis - the defeat of the small intestine.
- Gastritis - inflammation of various parts of the surface of the stomach.
- Colitis - the defeat of the walls of the large intestine.
- Enterocolitis - inflammation simultaneously affects several intestinal sections.
- Gastroduodenitis - simultaneous damage to the duodenum and the surface of the stomach.
All of the above diseases are observed in acute form. Intestinal infection becomes a provoking factor.
Classification and pathogens
The classification of intestinal infections is compiled according to the type of microorganisms that caused the disease. Allocate: 
- Bacterial Bacteria become pathogens. They are pathogenic or opportunistic. The first are microorganisms that should not be contained in the human body. When infected, they immediately provoke the development of inflammation. Conditionally pathogenic bacteria live in each person’s body. But under certain conditions, their active reproduction occurs, which starts the inflammatory process. Intrusion into the body of dangerous microflora occurs in violation of the principles of hygiene, as well as the use of infected food and water.
- Viral. Inflammation occurs due to the activity of viruses. Infection occurs oral, domestic or airborne method. The likelihood of such an infection is much higher than the bacterial one. A veteran person becomes a carrier of the virus. It is dangerous to others for two to three weeks after treatment.
- Protozoic. There are rarely enough. Infection occurs when swallowed dirty water from infected reservoirs. The treatment is quite long and requires the use of specialized drugs.
Depending on the type of disease, treatment programs may vary somewhat. Therefore, before starting treatment, it is necessary to determine the causative agent.
Causative agents of bacterial infection
Names and types of intestinal infections often occur from the name of the pathogen. Based on the infection rate, the list bacterial diseases are headed: 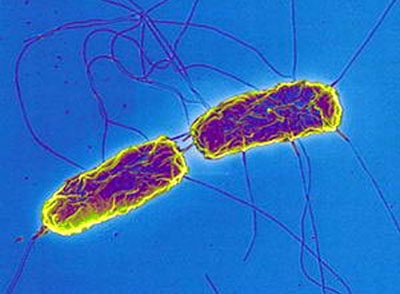
- Escherichiosis. The disease is caused by the activity of Escherichia coli. A rapid bowel failure occurs. Most often this problem is observed in young children.. Bacteria do not lose activity for several months.
- Dysentery. The cause of intoxication becomes the vital activity of bacteria belonging to the Shigella genus. As they die off, a large amount of toxin is produced in the human body. Dysentery is transmitted through contact with an infected person or after consuming contaminated water or food.
- Typhoid fever. Microorganisms enter the human body with water and food. As the disease progresses, there is an increase in lesions in the intestine, ulcers and wall ruptures are formed. The danger of the disease is also in the fact that incubation period can reach two weeks.
- Salmonellosis. The causative agent is Salmonella bacterium. Infection most often occurs after eating poor-quality meat, butter, eggs or milk. Hard to endure in childhood. It can lead to serious complications, such as swelling of the brain or renal failure.
- Cholera. The causative agent becomes cholera vibrio. During the illness, there is a strong dehydration due to incessant diarrhea and vomiting. Frequent cases of death.
- Brucellosis. Brucella intoxication leads to the defeat of not only the digestive tract, but also the musculoskeletal, sexual and nervous systems. Most often, the infection occurs after consuming low-quality dairy products. Microorganisms are not transmitted from person to person.
- Helicobacter pyloriosis. Exposure to Helicobacter pylori leads to severe damage to the duodenum and other parts of the digestive system. Ulcers may form on the mucous walls.
- Botulism. It's deadly dangerous disease caused by botulinum toxin. Microorganisms multiply in the absence of oxygen. Therefore, the source of infection is often homemade canned food cooked in violation of technology.
- Staphylococcus. Caused by bacteria of the same name as conditionally pathogenic. Slow development of the disease is often confused with a cold. Improper treatment leads to complications.
Causative agents of bacterial intestinal infections multiply rapidly in the human body. With the wrong or untimely treatment of such diseases, serious complications develop. Therefore, at the first symptoms, it is necessary to seek help from a doctor.
Viral infections
Viral infection of the gastrointestinal tract is no less dangerous than bacterial. There are several types of it: 
- Enterovirus. Observed in acute form. The first to be affected are muscular and nervous systems, a heart.
- Enteral hepatitis A and E. Infection occurs when drinking substandard water, eating infected products, or using dirty dishes.
- Rotavirus gastroenteritis. This disease is also called intestinal flu. Infection can occur through contact with a sick person. Therefore, in close contact with a large number of people, for example, in a school or kindergarten, an epidemic is often observed.
The treatment of such diseases should be carried out under the mandatory supervision of a physician.. Remember that self-medication can adversely affect your health.
Protozoal infections
The following types of disease are distinguished:  Amebiasis - infection with amoebas. First of all, the large intestine is affected. The development of abscesses in various internal organs. Infection through water, food, or interaction with a sick person.
Amebiasis - infection with amoebas. First of all, the large intestine is affected. The development of abscesses in various internal organs. Infection through water, food, or interaction with a sick person.
- Toxoplasmosis. Caused by Toxoplasma - microorganisms that live in the cells of the body of a person or animal.
- Giardiasis. The causative agent is Giardia. They lodge in the human small intestine. The disease develops as an enteritis. With late treatment, protozoa spread throughout the body..
- Balantidiasis. It is called the vital activity of the balantidial infusoria. Accompanied by the development of ulcerative colitis.
It is possible to detect the presence of microorganisms in the human body by analyzing urine, feces or vomit. Immunity to such diseases is not produced..
Symptoms of the disease
The main manifestations and symptoms of acute intestinal infections are similar. First, the disease may be asymptomatic. But more often, the symptoms appear quite sharply. First appear: 
- Pain in the abdomen, which are paroxysmal in nature. The duration of one attack can reach four minutes.
- Decreased appetite.
- Diarrhea. This symptom should be stopped as soon as possible. Long-term diarrhea often causes serious dehydration.
- Trouble sleeping
- Rash on the skin.
- Attacks of nausea, vomiting.
- Loud noises in the abdomen.
- Fatigue, drowsiness.
- Increased temperature in acute intestinal infection is quite often.
Depending on the pathogen that started the disease, there are a number of specific symptoms. Intestinal infection syndrome manifests itself as one of the following problems:
- Gastritic syndrome. Accompanied by pain, localized in the stomach, incessant nausea and vomiting after each meal.
- Gastroenteric syndrome. Unpleasant sensations concentrated in the navel, vomiting appears, fecal masses become greenish, they can detect mucus or blood impurities.
- Enteritic syndrome. The main symptom is frequent watery stools that are not accompanied by nausea or vomiting. Most often, this course of the disease is observed with cholera.
- Enterocolitic syndrome. Characterized by severe pain in abdomen, with urging to stool. Such symptoms are characteristic of dysentery or salmonellosis.
- Colitis syndrome. Pain is localized in the lower abdomen. There are traces of mucus and blood in the feces. False urges to defecate may appear.
Bacterial intestinal infection has symptoms of dehydration.. This is a dangerous condition that, if left untreated, is fatal.
Features of the course of the disease in childhood
Intestinal infections in childhood are quite common. The course of the disease is accompanied by bright symptoms. Infection most often occurs through poor-quality drinking water, infant formula, dirty fruits and vegetables.. In some cases, the child becomes ill after contact with an infected person. Most often, children suffer from the following diseases: 
- Enterovirus.
- Salmonellosis.
- Rotavirus infection.
- Dysentery.
- Escherichiosis.
The first signs of an intestinal infection: pain sensations in the tummy area, fever, and emetic urge. In fecal masses traces of mucus and blood are found. Dehydration is manifested by thirst, a decrease in urine volume and dry mucous membranes. With a long stay in this state, there is a weakness, excessive sleepiness.
If the baby's body temperature has risen to the level of 39 degrees, it is necessary to immediately consult a doctor. In addition to taking medication, treatment will include adherence to a special diet.
What complications can a disease cause?
If therapy was delayed or the degree of intoxication was significant, complications may develop. Among them are: 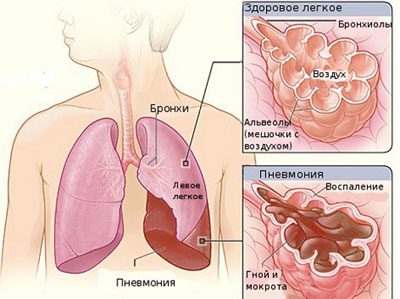
- Infectious toxic shock. It manifests itself shortly after infection. Its cause is an increased concentration of toxic substances in the body.
- Dehydration. Occurs due to prolonged diarrhea and vomiting. If dehydration reaches a critical point, a person may fall into a coma, after which death will occur. Signs of a problem are: a long absence of urination, dry mucous membranes, rapid heartbeat, low blood pressure, discoloration of the skin.
- Acute renal failure. May develop under the influence of toxins or be caused by dehydration..
- Pneumonia. Often occurs in children. Develops on the background of partial dehydration.
If an intestinal infection has led to such complications, long-term complicated treatment will be required.
What not to do if you suspect an intestinal infection
Often people, suspecting an infection in their intestines, are trying to cope with it on their own. Such self-medication can not pass without a trace and often leads to complications. Remember a few activities that are prohibited for this disease: 
- Eliminate pain with painkillers. This will make it difficult to accurately diagnose and develop a treatment program..
- Use fixatives without a doctor's prescription. With acute infectious disease toxins accumulate in the intestines. Diarrhea helps the body to clear. Taking such medications at this moment will trigger an increase in the concentration of toxins, which will aggravate the course of the disease.
- Apply to the stomach hot compresses. Heat enhances the inflammatory process..
- Apply folk or homeopathic remedies. Such techniques are permissible only as a supplement to conservative treatment after consultation with your doctor.
Only proper timely treatment with a preliminary medical examination can guarantee a successful recovery. Delay can threaten not only your health, but also life.
Correct diagnosis
In order to accurately determine the diagnosis and prepare a treatment program, the following measures are needed: 
- Collecting history. The physician should interview the victim for complaints. It is also necessary to find out the events that preceded the appearance of symptoms. Then the specialist examines the patient, evaluating his condition.
- A special rapid test will help identify the viral infection.. For its implementation, the test strip is immersed in human fecal masses. After 10 minutes, take the readings. If the result is negative, it is necessary to conduct tests for bacterial damage.
- Bacteriological examination allows to accurately determine the pathogen. It is carried out by planting samples of feces and vomit on a favorable environment. After several days, colonies of microorganisms are formed.
- Based on a blood test, serological testing is performed. It can be used to detect the presence of antibodies to microorganisms in the blood.
So simple and affordable. methods allow to detect pathogens with high accuracy. If signs of complications appear, the doctor additionally prescribes an instrumental examination, for example, colonoscopy, irrigoscopy or rectoromanoscopy. They help to determine the state of the digestive organs.
The basic principles of treatment
People often wonder if an intestinal infection can pass by itself. Specialist give a definite answer to this - no. The disease requires complex treatment.. Otherwise, the likelihood of serious complications. An individual therapy table is compiled for each patient. The principles of treatment are as follows: 
- Compliance with pastel and a certain diet. During an exacerbation, it is recommended to consume liquid food: vegetable soups, broths from low-fat meats, porridges. Boiled fish, steam omelette, baked peeled apples, cookies without baking are also allowed. It is strictly forbidden to use milk, smoked and fried foods, canned food, seasonings, onions, garlic, alcoholic beverages. Milk is not recommended to drink during the next three months after recovery.
- The use of specialized medicines. It includes the following directions:
- Treatment is primarily aimed at stopping the vital activity of pathogenic microorganisms. To do this, use antibiotics and intestinal antiseptics. The most commonly prescribed antibiotics are the fluoroquinolone group.
- At the same time it is necessary to take means to restore the normal intestinal microflora. These include probiotics: Linex, Hilak Forte, Acipol and others.
- Rehydration therapy helps to restore the water-salt balance. Together with adequate fluid intake, intravenous infusions of certain solutions are used.
- It is possible to clear the body of toxins with the help of sorbents: filtrum, enterosgel, smecta and others.
- Enzyme preparations: mezim, creon, pancreatin helps to establish normal digestion.
In severe cases, hospitalization of the victim may be necessary in a medical facility. If a disease is detected that is dangerous to others, then the patient is isolated. It is necessary to treat the disease under the supervision of specialists. The correct scheme of therapy is developed after a reliable determination of the pathogen..
Preventive actions
In order to minimize the chance of infection, the following guidelines should be followed: 
- Always follow the rules of personal hygiene. Try to wash your hands as often as possible.. If this is not possible, use antiseptic. This may be antibacterial wipes or a special gel for hands.
- To use only bottled or boiled water. Never drink from unknown sources and even more so reservoirs.
- Wash all fruits and vegetables thoroughly before drinking water. If you plan to feed the children, then you need to wash the fruit in boiled water. Do not be amiss to scald them with boiling water.
- Eat only well cooked meals. This is especially true of meat and fish.
- Perishable food must be stored in the refrigerator..
- Do not accumulate trash in the house. It can serve as a favorable breeding ground for bacteria. Try as often as possible to carry out wet cleaning in the house. Pay special attention to the sanitary condition of the bathroom and toilet. Increased humidity also contributes to the proliferation of bacteria.
Following these simple rules will help you forget about the problem, how to get rid of an intestinal infection. Always be attentive to your health and the foods you consume.
Remember that when the first symptoms of intoxication should immediately consult a doctor. Self-treatment in this case is unacceptable.
Popular
- What is the name of the Scottish skirt
- What women like a man archer
- Dosage and use of doxycycline when tick bite
- Sinupret - complete instructions
- Number of antennae in arachnid and insect crustaceans
- Help for enterobiasis for the pool, how much is valid
- Ceftriaxone suspension. What is ceftriaxone?
- Third degree breast cancer: prognosis and treatment
- Salt Scrub for the scalp
- Do girls how many centimeters to the uterus