What is ear otitis. Complications of acute otitis media
Many people know about the need to take care of their ears even from school when adults do not get tired of reminding children that they need to wear a hat and refrain from long walks in windy weather. Hypothermia dangerous development of a cold - and there and close to otitis. In fact, middle ear inflammation, or otitis media - this is often a secondary disease. It occurs against the background of respiratory infections, in most cases caused by bacterial infectious agents. The disease occurs with bright general symptoms, which are explained by intoxication of the body. In addition, with this disease, patients suffer from severe, sometimes unbearable earache, which is combined with intense headache.
In these cases, contraindications alternative - corticoid, administered directly through eardrum. The first reports of intratrampanic corticosteroids refer to the end of the decade. However, the procedure was not due to a contraindication of oral medication in patients with sudden deafness, but based on the hypothesis that injection at the site would increase the concentration of the drug inside inner ear and, therefore, have better results in its effect.
Based on this scientific body, the study showed that the administration of corticosteroids as an initial treatment, orally or intramuscularly, is only one of the options, signaling that there is no clear conclusion in the literature about its effect compared with placebo.
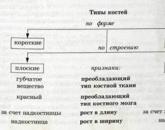
Classification
The middle ear is not a closed system. It communicates with the nasopharynx, as well as with the mastoid process. This makes it possible for infectious agents from the respiratory organs to enter the tympanic cavity. This way of infection is called tubar (tubogenic) and is implemented through auditory tube.
But this classification does not mean that the strategy of corticoids should be overlooked. If there is a chance of improving hearing through a systemic or intraparty corticosteroid, we should indicate this, because if the patient did not improve, we would have the only chance he had, says Dr. Mauricio Busle from the Iguazu Hospital, ENT specialist, Guidelines For example, the American Academy of Otorhinolaryngology, show the state of science at some point in history. Today, evidence of the existence of corticoids does not exist, so it can be prescribed; however, it should be remembered that the lack of evidence does not mean proof of invalidity, the guidelines are also important because they show gaps in knowledge and, therefore, are not law, but are a tool for directing their reasoning, Maurizio Kurk said.
Symptoms of otitis media vary depending on the variant of the pathological process. The exudate accumulating in the ear cavity is serous at first. It then becomes more viscous (catarrhal inflammation) and is subsequently transformed into purulent. At the same time in the initial period of inflammatory changes free exudate no. Acute lesions of the middle ear are classified as:
There are very few studies on spontaneous recovery in patients with sudden sensorineural hearing loss, but evidence suggests that this recovery can occur in about 65% of patients during the first 15 days. This proportion covers all possible degrees of loss: from mild to deep and even anacusial. Since subjects with more moderate losses do not apply for medical care and are those who tend to recover more easily and spontaneously, the percentage of people who see a doctor and who can register spontaneous improvement may be much lower, indicates Norma de Oliveira Penido. There is confusion in the literature, and from the moment we assume that sudden sensory loss is an emergency, we must take action; thus, we don’t know how many of them evolve spontaneously, although milder cases do not go to participate, he explains.
- tubootitis;
- purulent otitis;
- mycotic otitis
Adhesive, purulent, and they also speak at the mention of chronic forms.
With scarlet or measles infection, necrotic changes in the eardrum are observed, and there is also a high probability of otitis chronicity.
Tubo-otitis is otitis media, the symptoms in adults in which are explained by the localization of inflammation in the auditory tube and the tympanic cavity. When tubootitis in the cavity does not accumulate inflammatory effusion (or there is a meager serous exudate), but there is a tubular dysfunction. 
Only one option, when it is used as a primary treatment, an intraparty corticosteroid receives the status of a recommendation when considered in the context of rescue therapy. That is, according to the American leadership, it should be offered to patients who are not sufficiently restored after the initial strategy, which can be a systemic corticosteroid or observation, relying on the likelihood of spontaneous recovery. Three of the four randomized studies included in the guidelines consider intraparty corticosteroids to improve hearing, not placebo, and this improvement occurred in 53% to 90% of patients.
The defeat in tubootitis can be bilateral, accompanied by the occurrence of hearing loss.
The sensation of hearing loss with nasal congestion is familiar to many patients. When tubootitis patient hears constant noise in the ear. Hearing returns after the discharge of the nasal cavity from discharge (blowing out), administration vasoconstrictor drugs to improve nasal breathing - and worsens with re-accumulation of mucus and an increase in edema. Temporary relief comes while yawning. Symptoms are simultaneous. respiratory infection, the appearance of complaints of hearing loss on the background of a pronounced runny nose.
Intratipanic corticosteroid has no side effects, such as systemic, especially when it is contraindicated, and we know from studies of hearing preservation in cochlear implants that a corticosteroid absorbed by the inner ear prevents hearing loss, says Mauricio Busle. Ideally, this strategy should be implemented approximately 20 days after oral corticosteroid. Poured into the middle ear, the corticoid is absorbed through a round window to the inner ear.
The patient may complain of burning and dizziness, which can be minimized by slightly warming the corticoid, the doctor says. The procedure is repeated weekly through the ventilation tube for three weeks, always in the surgical center, as the patient must place his head by 45 degrees to maximize the entry of the corticosteroid into the round window. The procedure can also be performed under local anesthesia without sedation and without placing a vent.
Serous otitis
Serous inflammation of the middle ear is not accompanied by severe intoxication syndrome. Among the complaints of patients is not always marked pain, fever and weakness; in case of a rise in temperature, subfebrile indicators are observed.
How does middle ear inflammation manifest? Symptoms in an adult include:
- reduced hearing acuity;
- the appearance of noise in the ear, acquiring a permanent character;
- feeling of "fullness", "pressure" in the ear;
- "Splash" that occurs at the time of turning the head.
Hearing loss increases gradually, often very slowly. The anatomical integrity of the eardrum is preserved.
Methylprednisolone was the first corticosteroid to be tested on animal models. Since no more than 1 ml can be administered, the amount of product effectively administered when used at this concentration is lower. Thus, in Brazil, dexamethasone manipulation is necessary to obtain doses of higher concentration and brings with it the inevitable risks of error in this manual mode. Few pharmacies do this manipulation, and the doses produced in this way are nothing more than a product with a label without considering other problems, such as cost, shelf life, and product maintenance, explains Norma de Oliveira Penido.
During the change in the position of the head with the appearance of a “splash”, the hearing improves for a short time.
The predominant variant of the course of serous otitis media are oligosymptomatic "silent" forms. The absence of sudden bright changes (including pain syndrome), especially in case of unilateral damage, causes the symptoms of middle ear inflammation in adults to be detected late.
Although studies show that methylprednisolone is less absorbed by sensor cells and more painful than dexamethasone, the lack of a standardized product at higher concentrations makes the former a more convenient choice. 
The literature for this procedure shows a wide variety in dose, concentration, frequency, and number of injections. Thus, it is almost impossible to compare the results between jobs and determine the best way performing intratampic infiltration of corticoids, which, after all, is granted to a minority of patients.
Symptoms of otitis media in adults with purulent inflammation are characterized, above all, by intense pain. Pain syndrome is one of the leading manifestations - often it causes the patient to seek medical help. The description of pain can vary: someone  speaks of stabbing or shooting pain, someone complains of throbbing, excruciating incessant pain.
speaks of stabbing or shooting pain, someone complains of throbbing, excruciating incessant pain.
In the sudden deaf ambulatory hospital of São Paulo, out of 400 cases of sudden deafness, just over 20 patients underwent intraparty therapy. To date, there are no recommendations regarding the correct dose, but this is usually done with a single injection per week. Since we require adherence to auditory recovery criteria, we do two, because recovering 10 or 12 dB may not be enough for the patient, and in the case of rescue therapy, we perform the procedure because we want to get more than we do with an oral corticosteroid. Norma de Oliveira Penido.
How to understand that the patient? Symptoms are much more pronounced than in the cases described above. Of course, we can not exclude the likelihood of an atypical course (absence of fever, severe pain, or, conversely, severe intoxication, the presence of not only pain, but also nausea, vomiting, and intolerable headache). However, the following are most likely to occur:
Another lack of uniformity relates to the measurement of auditory recovery, regardless of whether it is consistent with oral or intraparty corticoid. Part of the work reviewed in the case of intrauterine therapy evaluates this recovery as a percentage of hearing improvement, assessed by pure tone, and sometimes with word recognition scores, which suggests that speech recognition tests were applied before therapy.
Only audiometric criteria are insufficient as improvement of threshold values has different influence depending on the recorded loss. A 10 dB recovery can affect people with moderate or moderate losses and not affect the lives of people with deep losses. In case of total loss, if the threshold returns to 60 or 50 dB, the redemption is partial, but the auditory gain is huge and the patient can use this social hearing with a hearing aid and may not even need technology if the return threshold is up to 40 dB.
- fever, general malaise;
- headache, lack of appetite;
- feeling of "overflow", noise in the ear.
When purulent otitis media worsens hearing - this is an important differential diagnostic character.
The occurrence of suppuration (otorrhea) is observed some time after the onset of the disease and is explained by the perforation of the eardrum, through the opening in which auditory canal pus enters. The duration of the perforated stage is several days (up to a week). At the same time, an abundant amount of pus that does not have a specific unpleasant odor is released. Over time, the volume purulent discharge decreases until the termination of otorrhea.
According to Norma de Oliveira Penido, there is a tendency to believe that salvation must reach the 50 dB threshold, since speech must be available and the subject will be able to register 50% of the discrimination. These criteria need to be assessed and discussed in our outpatient clinic; we have adopted an improvement criterion with four levels: full recovery when the threshold reaches the level of the contralateral ear; essential when it reaches the threshold of speech; partial irrelevance when it remains below this threshold, while the latter group brings together patients for whom there is no evolution of the situation or, worse, rarely but happens, he explains.
Chronic otitis
Chronic suppurative otitis media occurs by for various reasonsHowever, the delayed initiation of therapy, the wrong selection of drugs is essential. There are several forms of the disease, while doctors most often turn to the following classification:
- Mesotympanic.
- Epitimpanit.
- Epimesotympanitis.
The patient complains of symptoms such as:
The literature has shown that intraparty corticosteroids as a rescue therapy provide consistent benefits for some additional degrees of auditory recovery. He cannot but offer this therapy to a patient who has not recovered enough, either with observation or with other treatment options, because the literature shows the percentage of improvement, and it is worth noting that they are not necessarily treated earlier than they had a more pronounced improvement - says Maurizio Kurk.
Because in the end, an option or recommendation, administering corticosteroids with intra-park therapy is not a wonderful treatment, and we must remember that side effectssuch as pain, dizziness, drum perforation and even hearing impairment. When internal treatment began, we thought it would be a solution, but it is not so simple. In certain situations, this may be the best option, but it must be very well indicated to understand where the best efficacy will be and when patients will benefit, says Norma de Oliveira Penido.
- discharge from the ears (purulent, mucopurulent character);
- feeling of pain, "aches", "filling" the ear;
- headache occurring on the affected side;
- hearing impairment, ear noise.
Allocations are noted periodically or permanently. In the acute period, they become abundant, the clinical picture is complemented by increased pain (and local in the ear, and headache), dizziness. Fever may occur.
Oral or intrauterine therapy with corticosteroids for idiopathic sudden sensorineural hearing loss: a randomized study. Viruses, bacteria and inflammation can cause hearing loss. It is clear that ear inflammation can impair hearing, but diseases such as scarlet fever, measles and meningitis can also lead to hearing loss. This type of disorder is also associated with viral and bacterial lesions, which are otosclerosis, which affects the bones of the ear.
Many infections can cause severe or chronic hearing loss. Although cooling is usually harmless, more than one hundred variants of cold-causing viruses that can cause otitis interns, otitis or otitis from influenza are known. These disorders can cause deafness.
Mesotympanic mania is manifested by the periodic release of mucous or mucopurulent masses that do not have an unpleasant odor. There is also noise in the ear, dizziness. During the period of exacerbation, pain syndrome, fever, a sharp increase in the amount of secretions, increased headache. Patients may experience nausea, vomiting. In addition, dizziness becomes stronger.
Acute otitis media is one of the most common infections of the auditory system. It occurs most often during viral or bacterial infection upper respiratory tractsuch as cold or chill. Inflammation extends to the middle ear with an Eustachian tube. Common symptoms of otitis media are throbbing and throbbing pain in the ears, fever and deafness. In most cases, acute otitis media can be cured only with antibiotics. In case of complications or particular forms, it can permanently damage your hearing.
In all cases, in the presence of otitis media and other infectious diseases, it is strongly recommended to consult with your doctor so that he establishes a diagnosis based. The ear is the organ of the most fascinating feeling, which plays not only a well-known auditory function, but is also a fundamental component of the equilibrium apparatus. The system consists of a part dedicated to hearing, in which nature has organized the ideal mechanism of mechanoelectric transduction; and one in which highly specialized sensors capture the movement of our body.
Epitimpanitis is characterized by damage not only of the mucous membrane, but also of bone tissue. Named Form chronic otitis runs hard, may be accompanied by the formation of cholesteatoma. Patients are worried about the presence of discharge with an unpleasant smell, sometimes having the appearance of "crumbs" or containing blood. Abundant suppuration is observed on the background. elevated temperature body weakness, dizziness.
Epimesotimpanitis combines the symptoms of each of the above variants of the disease. When epimesympanitis on the radiograph can be observed signs of destruction of the temporal bone. 
The function of hearing deteriorates in all forms of chronic otitis, but the impairment is most pronounced in epimesympanitis.
Mycotic otitis (otomycosis)
Infection of the fungal nature in the event of damage to the middle ear often becomes secondary. Otomycosis occurs on the background of a chronic course of an already existing purulent process. Otomycosis is not necessarily candidiasis (that is, an infection caused by yeast-like fungi of the genus Candida). It can also be provoked by mold fungi belonging to the genus Penicillum, Mucor, Aspergillus. Inflammation of the middle ear, the symptoms of which are caused by a fungal infection, can be described in the table below:
| Infection option | Patient complaints | Objective symptoms |
| Aspergillosis | the presence of abundant pathological discharge; intense itching of persistent or periodic nature; feeling of "fullness", ear congestion, noise in the ear; headache concentrated in the area of the affected ear. |
Discharge (often plaque) gray with black splashes, black, brown color. Powdered discharge yellowish with unpleasant pungent odor. |
| Candidiasis | Cheesy mass of watery consistency, whitish hue. | |
| Mukoroz | Detachable looks like a "fluffy raid", can be compared when describing with felt. It has an unpleasant smell of mold. |
Mycotic otitis may be accompanied by severe pain - this is due to the defeat of the deep layers of the skin.
Fungal lesion of the middle ear is usually combined with mycotic infection of the ear canal. Average otomycoses are characterized by a long protracted course, periodic exacerbations. Hearing loss due to the accumulation of fungal mycelium in the ear canal.
The infection can be one-sided or affect both ears - the patient himself sometimes contributes to its spread when the ear toilet is improperly carried out, and it is necessary to scratch it. Otitis media of the middle ear, the symptoms of which occur from time to time in the presence of a chronic purulent process and include a pronounced, severely tolerated itching by the patient - an indication for examination regarding mycotic infection.
Otitis is the general definition of various inflammatory diseases ear.
Middle ear - is a system of air cavities, including: the tympanic cavity, the auditory tube, the entrance to the cave, mastoid cave and mastoid cells opening into it.
In inflammatory diseases of the middle ear, all its departments are usually involved in the pathological process, but the severity and localization of disorders in various diseases differ. An important role in the pathology is played by the topographic-anatomical features of the middle ear.
The upper bone wall of the tympanic cavity and mastoid cave is adjacent to the bottom of the middle cranial fossa, where the temporal lobe of the brain is located. In this bone plate in adults, there are devisations, and in children of the first years of life, on the border of the stony and scaly parts of the temporal bone in the roof of the tympanic cavity there is an open stony-scaly gap (fissura petrosquamosa). The contact of the mucous membrane of the middle ear with the dura mater makes it possible to spread the infection into the cranial cavity.
The medial (labyrinth, promontory) wall separates the tympanic cavity from the inner ear, here are the windows of the vestibule and the cochlea. Through the membranous formations of labyrinth windows, the infection can penetrate into inner ear and cause the development of labyrinthitis.
 Here, on the medial wall, in the bone bed is a canal facial nerve (canalis p. facialis) in which his horizontal knee passes. The defeat of the facial nerve (paresis or even paralysis) in various forms of otitis can occur due to exposure to microbial toxins, direct compression of the nerve or even destruction of its trunk by cholesteatoma.
Here, on the medial wall, in the bone bed is a canal facial nerve (canalis p. facialis) in which his horizontal knee passes. The defeat of the facial nerve (paresis or even paralysis) in various forms of otitis can occur due to exposure to microbial toxins, direct compression of the nerve or even destruction of its trunk by cholesteatoma.
The posterior part of the middle ear is represented by the mastoid process (processus mastoideus), in which there are numerous air cells connected to the tympanic cavity of the mastoid antrum (antrum mastoideum). Mastoid cave - airy cell of a rounded shape, which is constantly present in the mastoid process, regardless of its shape and structure. This is a reliable anatomical landmark for ear surgery. In children of the first year of life, the mastoid process is not developed, but the mastoid cave is already present at birth. In newborns, it is located superficially (at a depth of 2 to 4 mm) and slightly above the ear canal. Development mastoid the child begins in the 2nd year of life and ends by the beginning of the 7th year, with the cave gradually moving backwards and downwards.
Depending on the number, size and location of the cells in the mastoid process, there are several types of its structure: pneumatic, diplomatic and sclerotic. The nature of the emerging pathology largely depends on the nature of the structure of the mastoid process. So, with its sclerotic structure, an underdeveloped mastoid is formed in a person who has suffered from chronic purulent otitis media since childhood; with the pneumatic structure of the process, the likelihood of mastoiditis is higher.
Adjacent to the posterior surface of the mastoid process is the sigmoid sinus (sinus sigmoideus), the venous sinus through which blood flows from the brain to the jugular vein system. Under the bottom of the tympanic cavity, the sigmoid sinus forms an extension — the bulb of the internal jugular vein. The sine is delimited from the cellular system of the mastoid process by a thin but rather dense bone plate (lamina vitrea). A destructive inflammatory process that develops in the mastoid process in some diseases of the middle ear can lead to the destruction of this lamina and the penetration of infection into the sinus and posterior cranial fossa.
The front wall of the tympanic cavity is called the tubular, or carotid, wall (paries tubaria s. Caroticus). The upper half of this wall is occupied by two openings, most of which are called the tympanic mouth of the auditory tube (ostium tympanicum tubae auditivae). Above it opens the floor of the muscle channel, tightening the eardrum (t. Tensor tympani). In the lower section, the anterior wall is formed by a thin bone plate separating the tympanic cavity from the trunk of the internal carotid artery, which passes through the channel of the same name. This wall is penetrated by thin canaliculi through which the inflammatory process can pass from the tympanic cavity to the carotid artery.
The mucous membrane of the tympanic cavity is a continuation of the mucous membrane of the nasopharynx and is represented by a single-layer flat and transitional ciliated epithelium with few goblet cells. Covering the auditory ossicles and ligaments, the mucous membrane forms many communicating pockets and sinuses, among which the clinically most important are the tympanic and facial sinuses. The drum sinus (sinus tympani) is under the pyramidal elevation and extends to the bulb of the jugular vein and the window of the cochlea. The facial sinus (sinus facialis) is limited to the medial canal of the facial nerve, to the rear - to the pyramidal elevation and to the front - to the cape.
Inflammation of the outer earoften occurs due to infection and affects the skin of the outer ear, which includes not only the visible ear, but also part of the ear canal leading to the inner parts of the ear. Sometimes inflammation is localized. Although inflammation can be painful and unpleasant, it is often well treatable. However, in patients with diabetes, the elderly and people with a weakened immune system, the disease can lead to malignant otitis of the outer ear, a rare non-carcinogenic (despite its name) disease.
The reasons
Moisture in the ear contributes to the development of fungal and some types of bacterial infectious diseases. Swimming, especially in polluted water, increases the risk of otitis of the outer ear; bathing in the shower, washing your hair or being in the rain do not practically increase the risk of disease.
Skin diseases, such as eczema or seborrheic dermatitis, can cause inflammation.
Objects inserted into the ear, such as cotton swabs, can create small cuts that are vulnerable to infection.
Excessive production of sulfur makes the ear more vulnerable to infection.
Means for removing sulfur, hair dye, shampoos, polishes or chlorinated water can irritate the ear canal.
Diagnostics
The doctor examines the ear canal with an otoscope. An assay for sowing fluid from the ear can be made.
Symptoms
Itching in the ear canal on early stages.
Pain in the ear that can become severe. The ear becomes sensitive to touch, and the pain worsens when you pull it back. auricle.
Discharge of fluid or pus from the ear canal.
Redness and swelling of the skin of the ear canal (and sometimes the outer ear), which leads to blockage of the ear canal.
A small, painful lump or boil in the ear canal.
Temporary hearing loss due to swelling and accumulation of pus in the ear canal.
Fever.
Treatment
You can take over-the-counter pain relievers. Children should take acetaminophen, not aspirin.
Your doctor may use a small aspirator to remove fluid and pus from the ear canal.
Antibiotics or antifungal ear drops may be prescribed to fight infection; in addition to them, corticosteroids are used to reduce inflammation. A sponge-like wick can be inserted into the ear so that medications penetrate deep into the ear canal.
With a strong infection, oral antibiotics are possible.
Surgical removal of dead tissue may be necessary in the treatment of severe otitis of the outer ear.
Codeine or drugs can be prescribed to reduce severe pain.
After the symptoms disappear, avoid getting water into the ear canal for three weeks; protect your ears when you shower and do not swim.
If the disease recurs, continue using the prescribed ear drops to ease the symptoms.
Consult your doctor if symptoms persist for more than one to two days. (People with diabetes should see a doctor at the first sign of an ear infection.)
Prevention
Do not insert into the ear any objects, even cotton swabs, and do not clean the ear with alcohol or non-prescription solutions. Your doctor may remove sulfur.
If you often experience itching in the ear canal, consult your doctor. Treatment of skin disease will help prevent secondary infection.
Avoid swimming in water that may be contaminated.
If you floated in water that could cause otitis of the outer ear, wash your ears with water acidified with vinegar; It may prevent infection.
Acute inflammatory diseases of the middle ear
The predominant development of pathological changes in a given division of the middle ear determines the existence of various nosological forms of the disease. Thus, the localization of disorders mainly in the auditory tube is interpreted as Eustachitis or catarrhal otitis media; inflammation, which has developed predominantly in the tympanic cavity, is designated by the term "otitis media", and the pathology in the mastoid cave and adjacent cells is called mastoiditis.
Diseases of the middle ear are rarely primary. An important role in their development is played by dysfunction of the auditory tube, which is usually a reflection of pathological changes in the upper respiratory tract. Therefore, therapeutic measures are aimed primarily at restoring the normal functioning of the auditory tube.
Due to the peculiarities of the anatomical and morphological structure of the middle ear, the inflammatory changes that develop in it are characterized by the predominance of the exudative form of inflammation, in which the reactions of the microcirculation system prevail over the processes of alteration and proliferation. The amount of protein and the cellular composition of the exudate can vary depending on the degree of violation of vascular permeability.
Among different types exudative inflammation of the mucous membrane of the middle ear are most common catarrhal, serous and purulent.
Middle ear inflammation - This is a disease of the cavity between the eardrum and the thin structures of the inner ear. It usually occurs when viruses, causing disease upper respiratory tract (for example, runny nose), or bacteria migrate through the Eustachian tube (the passage between the nasal canals and the middle ear). Infection often leads to blockage of the tube, making it difficult for mucus, pus, and other fluids produced during an illness to leak from the middle ear. It hurts because these fluids put pressure on the eardrum and can break it. Middle ear infections are very common in children (because they have a smaller Eustachian tube) and have a tendency to recur, especially in winter. With fast treatment There are all possibilities for full recovery. If untreated, chronic otitis media can eventually cause a serious structural impairment of the ear and skull, which results in irreversible hearing loss or weakness of the facial nerve.
The reasons
Viral infection of the upper respiratory tract is the most common cause.
Allergic rhinitis or adenoids can cause blockage of the Eustachian tube.
A torn eardrum makes it easier for carriers of an infection to enter the middle ear.
Children with congenital anatomical defects of the face (such as “cleft lip”) or children with the syndrome
Down's are at greater risk of middle ear infections.
Some groups of people have a hereditary predisposition to infectious diseases of the ear.
Passive smoking increases the risk of middle ear infections in children.
Repeated bacterial ear diseases can result in chronic inflammation of the middle ear.
Symptoms
The feeling of fullness of the ear, which ultimately leads to severe pain.
Temporary hearing loss in a sore ear.
Fever.
Dizziness.
Nausea and vomiting.
Clicks or other sounds in the ear when moving the jaw.
Back pain in the auricle.
Continuous discharge of pus and moderate hearing loss are often without earache (the primary signs of chronic middle ear inflammation).
Diagnostics
The physician should examine the ear canal with an otoscope - a small instrument with light. An assay for sowing fluid from the ear can be made.
Treatment
Antibiotics may be needed to treat a bacterial infection.
Aspirin or acetaminophen is taken to ease pain and fever.
A small incision can be made in the eardrum (myringotomy) to release pus. This incision heals in two to three weeks. With myringotomy, a tube can be inserted to drain the middle ear during fluid accumulation.
Enlarged adenoids can be surgically removed.
Sometimes an infectious disease affects the mastoid bone (bone behind the ear), which must be surgically removed.
See your doctor if you or your child feel an earache that persists despite the treatment, especially if the symptoms worsen or are accompanied by swelling around the ear, twitching of the face, or severe ear pain that suddenly stops (which indicates rupture of the eardrum) .
Prevention
Washing hands with soap warm water should be mandatory for both children and adults in schools and kindergartens.
At home, regularly wash bed linens, towels, and heating pads to prevent re-infection from residual pus. Throw cotton balls away after use.
Acute catarrhal otitis media
Catarrhal inflammation of the mucous membrane of the middle ear, developed as a result of dysfunction of the auditory tube, is denoted by the term "tubo-otitis", or "eustachitis." There is usually no free effusion in the tympanic cavity of this disease. The main role is played by the pathological process in the auditory tube, which leads to a breakdown of its functions, impaired ventilation of the tympanic cavity and moderate inflammation in the latter. Infection of the mucous membrane of the auditory tube occurs during acute respiratory diseases, influenza, and in children with acute infectious diseases, accompanied by catarrh of the upper respiratory tract. The causative agents of tubotitis are viruses, streptococci, staphylococci, etc.
Tubar dysfunction is more persistent with adenoid vegetations, various chronic diseases nasal cavity and paranasal sinuses (chronic purulent or polypous rhinosinusitis, choanal polyps, curvature of the nasal septum, hypertrophy of the posterior ends of the inferior nasal conchs, etc.), as well as nasopharyngeal tumors. The cause of some forms of tubotite can be abrupt changes in atmospheric pressure during the ascent and descent of the aircraft (aerootite), during the diving and ascent of divers and submariners (mareotite).
In case of violation of the ventilation of the tympanic cavity, the air contained in it is sucked up by the mucous membrane, and the replenishment of the air reserve is difficult due to the compression of the mouth of the pipe. As a result, the pressure in the tympanic cavity drops, the air in it becomes rarefied. In this case, the tympanic membrane retracts, and transudate may appear in the tympanic cavity.
Clinic. A patient with tubootitis complains of a feeling of ear congestion, a decrease in hearing, sometimes a noise in the ear, autophony (resonance of one's own voice in the diseased ear). Ear bumps may appear during an acute respiratory viral infection or during the recovery period after it, as well as after suffering an atmospheric pressure differential, for example, after flying in an airplane. The pain in the ear is usually absent or slightly expressed, the general condition suffers a little.
Diagnostics. When otoscopy can be observed in the tympanic membrane, as indicated by the apparent shortening of the handle of the malleus, a sharp distance in the direction of the ear canal of the short process, more pronounced front and rear folds, the disappearance or deformation of the light cone. Sometimes radial injection of the tympanic membrane vessels along the handle of the malleus or circular injection of vessels in the annulus tympanicus area is determined.
Hearing in acute tubootitis is reduced slightly (to 20–30 dB) mainly due to a violation of the sound conduction at low frequencies. Sometimes patients notice an improvement in hearing after yawning or swallowing saliva, which is accompanied by the opening of the lumen of the auditory tube.
Treatment of tubotitis is primarily aimed at eliminating adverse factors affecting the state of the pharyngeal mouth of the auditory tube. To reduce the swelling of the mucous membrane in this area, the patient is prescribed vasoconstrictor drops in the nose (naphthyzin, sanorin, tezin, nazivin, etc.). Antihistamines (suprastin, astemizol, claritin, etc.) also contribute to the reduction of mucosal edema. In order to prevent the discharge of infected mucus from the nasopharynx through the auditory tube into the tympanic cavity, the patient should be warned against excessively vigorous blowing of nose.
In the presence of inflammatory changes in the nasopharynx, it is not necessary to purge the auditory tubes according to Politzer; preference is given to catheterization of the auditory tube, performed after careful anemisation of its pharyngeal mouth. Through a catheter into the lumen of the auditory tube, you can enter a few drops of 0.1% aqueous solution of adrenaline or dexamethasone. In complex therapeutic measures include various physiotherapeutic procedures: UFO, UHF on the nose, laser therapy to the area of the mouth of the auditory tube, pneumomassage of the eardrum.
Acute tubo-otitis with adequate treatment usually takes a few days. The effectiveness of therapy depends on the timely elimination of the pathology of the nasal cavity, the paranasal sinuses and the nasopharynx, which contribute to the development and support of the course of tubo-otitis.
Exudative otitis media
This disease develops against the background of dysfunction of the auditory tube and is characterized by the presence of serous-mucous effusion in the tympanic cavity.
The leading pathogenetic factor of exudative otitis media is persistent violation of the ventilation function of the auditory tube. The name of this form of the disease itself indicates an increased secretion of mucus and a protracted course. In this regard, characteristic features include the appearance in the tympanic cavity of a thick viscous secretion, a slowly increasing hearing loss and a prolonged absence of a defect of the eardrum.
Along with persistent tubular dysfunction, exudative otitis media is based on a change in the immunobiological properties of the organism, a decrease in general and local resistance. The reason may be transferred respiratory viral infection, unreasonably wide and irrational use of antibiotics. An important role is played by immunopathological reactions, which indicate the development of sensitization of the mucous membrane of the middle ear.
Given the dynamics inflammatory process and the corresponding pathological changes distinguish four stages of the disease.
Stage I - catarrhal. At this stage, due to the violation of the ventilation function of the auditory tube and the formation of negative pressure in the tympanic cavity, conditions are created in it for the emergence of transudate. A small number of neutrophilic leukocytes and lymphocytes migrate, the secretory elements show readiness for mucus release. At the same time, a tympanic membrane is detected clinically. Its color changes from cloudy to pink, there is a slight autophony, a slight decrease in hearing (air conduction thresholds do not exceed 20 dB, bone conduction thresholds remain normal). Duration catarrhal stage - up to one month.
Stage II - secretory. It is characterized by intensive secretion and accumulation of mucus in the tympanic cavity. Metaplasia of the mucous membrane of the middle ear develops with an increase in the number of secretory glands and goblet cells. Subjectively, this is manifested by a feeling of fullness and pressure in the ear, sometimes by noise in the ear and more pronounced conductive hearing loss (up to 20 - 30 dB). Often, the patient feels a transfusion in the ear fluid (splash) when the position of the head changes and at the same time notices an improvement in hearing. This can be explained by the fact that when the head is tilted, the fluid in the tympanic cavity moves, while the niches of the windows of the labyrinth are freed and hearing is improved.
When otoscopy note that the eardrum is retracted, its contours are expressed, the color depends on the contents of the tympanic cavity and varies from pale gray to bluish with a brownish tinge. Sometimes when otoscopy through the membrane, you can see the level of the liquid in the form of an arched line, which moves when the head position is changed. The duration of the secretory stage can be from 1 to 12 months.
Stage III - mucosal. This stage is distinguished by the fact that the contents of the tympanic cavity (and sometimes other middle ear cavities) become thick and viscous. At the same time, hearing loss increases (with thresholds up to 30-50 dB), in some cases bone marrow thresholds increase. If the entire tympanic cavity is filled with exudate, or if the latter becomes viscous and thick, the symptom of fluid movement disappears. To designate such otitis (with sticky, viscous contents in the tympanic cavity), some authors use the term “sticky ear”. The mucosal stage develops with a total disease duration of 12 to 24 months.
Stage IV - fibrous. It is characterized by the predominance of degenerative processes in the mucous membrane of the tympanic cavity. At the same time, the production of mucus decreases, and then completely stops, there comes a fibrous transformation of the mucous membrane with involvement in the process auditory ossicles. Progressing mixed hearing loss. The development of the cicatricial process in the tympanic cavity leads to the formation of adhesive otitis media.
Diagnostics. When diagnosing exudative otitis media, it is necessary to take into account factors that can cause tubular dysfunction. First of all, they study the nasal cavity in order to identify obvious abnormalities, such as deformation of the nasal septum, inflammatory changes in the paranasal sinuses, hypertrophy of the posterior ends of the inferior nasal concha, etc. Also take into account any changes in the architecture of the nasal cavity, accompanied by obstruction of the air flow on the inhale and exhale.
Otoscopy and otomikroskopiya allow us to estimate the color of the eardrum, its transparency, thickness, elasticity, mobility and vascularization. Tonal threshold audiometry reveals a violation of sound conduction in the area of speech frequencies and allows you to determine the bone-air gap to 30 - 40 dB.
A highly informative method for diagnosing this form of the disease is acoustic impedancemetry - measurement of the acoustic resistance (compliance) of the outer, middle and inner ear. The method allows to evaluate the elasticity of the eardrum, the level of pressure and the presence of exudate in the tympanic cavity, the function of the auditory tube.
Pathognomonic for exudative otitis media are type C tympanograms (which show a decrease in tympanogram peak height and a decrease in tympanal pressure) and type B (decrease in tympanogram amplitude sometimes to a horizontal line).
In the diagnosis of exudative otitis media, acoustic reflexometry is also used - registration of compliance of the sound-conducting apparatus while reducing the stapedial muscle. The threshold of the acoustic reflex is normally 80–100 dB. When conductive hearing loss acoustic reflex on the side of the patient ear is usually absent.
Treatment. The effectiveness of treatment of exudative otitis media is the higher, the earlier it is started. First of all, you should strive to restore the function of the auditory tube. This is achieved by the rehabilitation of inflammatory diseases of the nose, paranasal sinuses and pharynx.
In order to avoid infection of the tympanic cavity, irrigation of the nasal cavity by means of the physiomers or aqua maris and irrigation of the nasal and pharyngeal cavity with bioparox or polydex with phenylephrine is carried out. An important role is played by proper cleaning of the nasal cavity. The alternate (on the exhale) screening of each half of the nose should be carried out without tension.
Anemization of the pharyngeal mouth of the auditory tube is carried out as follows. A metal probe with a padded jacket moistened with a 0.1% adrenaline solution and a 10% lidocaine solution, for 5–10 s, is supplied to the pharyngeal orifice of the auditory tube. The procedure is repeated for 7-10 days.
To reduce edema of the mucous membrane and exudation in the nasal cavity, paranasal sinuses, auditory tube and the tympanic cavity with a short course (6-7 days), systemic decongestant, phenylephrine hydrochloride, is used. It is part of a number of combination drugs - rhinopront, coldrex, rinza.
In order to improve the tubular function, the ears are blown along Politzer or through an ear catheter with simultaneous massage of the eardrum with the help of a Siegle funnel. Dexamethasone, antibiotics, trypsin, chymotrypsin are injected through the catheter into the lumen of the auditory tube. Endaural electrophoresis with the introduction of proteolytic enzymes and lidz is quite effective. The appointment of antihistamines is recommended in cases where serous otitis media develops in the face of allergies.
In the acute stage of the disease, administration of glucocorticoids is shown, which have a pronounced anti-inflammatory effect, reduce exudation and tissue edema. Prednisolone is prescribed 30 mg orally or as an injection for 6 days. Fenspiride (Erespal) also has a pronounced anti-inflammatory effect, it is administered orally 80 mg 2 times a day for 10 days.
Showing tonic means, vitamins; Recently, immunocorrectors (for example, polyoxidonium, 0.006 g intramuscularly every other day, a total of 6-10 injections) have been increasingly included in the complex of therapeutic measures.
If the function of the auditory tube is not restored, the exudate is not absorbed and the hearing does not improve, surgical methods are used to evacuate secretions from the tympanic cavity. The most widely used bypass the tympanic cavity. An incision of the tympanic membrane is performed in its lower quadrant, and a shunt of a bioinert material — Teflon, silicone, and polyethylene — is inserted through the incision. There are many forms of shunts: a drainage tube with holes, a coil, a tube with a semi-permeable membrane, etc. Usually, drainage is left in the ear until recovery and improvement of the tubular function, i.e. from several weeks to 1-2 years.
Effective is the method of shunting through the subcutaneous tunnel formed in the region of the back wall of the auditory canal - transcutaneous (metotympanal) shunting of the tympanic cavity. Silicone drainage tube is held under annulus tympanicus, without damaging the eardrum. At the entrance to the ear canal it is fixed to the skin with a silk suture. Through this drainage tube, the secretion is aspirated from the tympanic cavity, various medications.
In some cases, exudative inflammation is not limited to the tympanic cavity, but extends to the antrum and cells of the mastoid process, and sometimes the mastoid entrance block develops. In this case, an antrotomy is performed, a drainage tube is inserted into the antrum and left for 2-4 weeks. Sometimes an antrotomy (intraocular approach) and intrameatal tympanotomy are performed simultaneously with the introduction of one drainage tube under the muscle-tympanic flap for a long time, and the other into the mastoid cave for 3–4 weeks.
It should be noted that the exudative otitis media in the initial stages does not always have vivid clinical manifestations, however, with a prolonged progressive course of the disease, the disease can lead to persistent hearing loss and cochleo vestibular disorders. Currently, there are highly informative methods for diagnosing exudative otitis media, which allow timely recognition of the disease and monitoring the effectiveness of its treatment.
Acute suppurative otitis media
This is an acute inflammation of the mucoperioste of the tympanic cavity, in which all parts of the middle ear are involved to some extent in the process. The disease is widespread, it can occur sometimes in a light form, then, rapidly developing, to cause severe overall inflammatory reaction of the body.
The cause of the disease is a combination of factors such as a decrease in local and general resistance and infection in the tympanic cavity. The main causative agents of acute otitis media (up to 80% of cases) in adults and children are S. pneumoniae and H. influenzae, more rarely M. catarhalis, S. pyogenes, S. aureus, or microbial associations (Fig. 8.8). Viral otitis often develops during epidemics viral diseases.
Penetration of infection into the tympanic cavity can occur in various ways: tubogenic, hematogenous, through the damaged eardrum when it is injured or through the mastoid wound, as a result of retrograde spread of the infection from the cranial cavity or from the labyrinth.
The most frequent route of infection is the tubogenic - through the auditory tube. The hematogenous pathway of infection in the middle ear is relatively rare, it is possible with such infectious diseases as influenza, scarlet fever, measles, typhoid, tuberculosis and others, and is usually associated with impaired resistance of the organism.
The main causative agents of acute otitis media
Haemophilus influenzae Streptococcus pneumoniae Streptococcus pyogenes Moraxella catarhalis OthersWhen an infection enters the middle ear through a damaged eardrum when it is injured or through a wound of the mastoid process, they speak of traumatic otitis media. In extremely rare cases, acute otitis media develops as a result of retrograde infection from the cranial cavity or from the labyrinth.
The main stages of the pathogenesis of acute otitis media with ARD are shown in Fig. 8.9. With inadequate treatment or other adverse conditions, the process can progress and from the usual acute catarrhal form go into the acute purulent form.
The main pathogenesis of acute suppurative otitis media.
Inflammation of the mucous membrane of the auditory tube and the tympanic cavity, edema, leukocyte infiltration. . Filling the cavities of the middle ear exudate, which initially is serous, and then becomes purulent. . As a result of strong pressure of purulent exudate and circulatory disorders, perforation of the eardrum occurs with the subsequent development of otorrhea. . Muco-purulent discharge gradually becomes thick purulent. As the inflammatory changes subside, their number decreases, and the suppuration stops completely. . Perforation of the eardrum can heal, but if it persists, the disease becomes chronic.
Clinic. Local and general symptoms of the disease are expressed differently depending on the stage and severity of the process.
There are 3 stages of acute purulent otitis media:
Pre-deferred; perforating; reparative.
Not in all cases the process necessarily goes through all three stages, in some cases the disease can acquire an abortive course already at the first stage.
The initial, pre-perforative, stage of the disease is characterized by pronounced local and general symptoms. The main complaint is pain in the ear, often very sharp, giving into the head, crown. Steadily growing, it sometimes becomes painful, unbearable. In some cases, pain is observed during palpation and percussion of the mastoid process, which is caused by inflammation of its mucosa. At the same time, as a result of inflammation and restriction of mobility of the eardrum and the chain of auditory ossicles, congestion and noise in the ear occur. During this period, the general condition of the patient is often disturbed — signs of intoxication appear, the body temperature rises to 38–39 ° C, and changes in the peripheral blood are characteristic of the inflammatory process.
When otoscopy is first visible injection of blood vessels along the malleus and radial vessels of the membrane, accompanied by a shortening of the light cone. Then the hyperemia of the tympanic membrane grows, becomes diffuse, its identification points disappear, the membrane bulges, becomes infiltrated (Fig. 8.10). The duration of the initial stage of acute otitis media is from several hours to 2 - 3 days.
Perforated stage is characterized by perforation of the eardrum and the appearance of suppuration. At the same time, the pain in the ear quickly subsides, the state of health improves, the body temperature decreases. The discharge from the ear is first abundant, mucopurulent. When otoscopy can be observed so-called "pulsating reflex", in which the pus enters through the perforation portions, synchronous pulse.
After a few days the amount of discharge decreases, they become thick and become purulent. Suppuration usually lasts 5 to 7 days. Perforation with acute otitis media is usually small, more extensive perforations are with scarlet, bark, tuberculous lesion.
The reparative stage is characterized not only by stopping the suppuration and (in most cases) spontaneous scarring of the perforation, but also by the restoration of hearing. Gradually decrease, and then the discharge stops, simultaneously the hyperemia and infiltration of the eardrum disappear, its luster appears, the identification contours become visible. Under normal immune status, sufficient function of the auditory tube and adequate treatment, recovery may occur, bypassing the perforative stage.
The duration of the disease usually does not exceed 2 - 3 weeks. However, the typical course of acute purulent otitis media can be disrupted at any stage of the process. Complicated course and adverse outcome of acute purulent otitis media may be due to a decrease in local and general immune defense of the body, high virulence of the pathogen and its resistance to antibiotics used, as well as irrational therapy.
Diagnosis in a typical course of acute suppurative otitis media is not difficult. The diagnosis is made on the basis of complaints, anamnesis and features of the otoscopic picture.
Treatment of a patient with acute purulent otitis media is carried out taking into account the stage of the disease, the severity of clinical symptoms and the peculiarities of the patient’s somatic status. In the acute stage of the disease, an outpatient regimen is recommended, and with a marked increase in temperature, general malaise - bed rest. If there is a suspicion of an incipient complication, the patient should be urgently hospitalized.
In order to restore or improve the ventilation and drainage functions of the auditory tube, vasoconstrictive drops (0.1% solution of naphthyzin, sanorin or galazolin) are prescribed, which are poured into 5 drops in the nose 3 times a day, preferably in the position of the patient "lying on his back .
Treatment in the preperforative stage. In severe otitis media with severe pain and fever up to 38 ° C and above, the prescription of antibiotics is shown in the preperformative stage. The drug of choice in the treatment of uncomplicated otitis media in adults is amoxicillin 0.5 g orally, 3 times a day for 7-10 days. If there is no effect after three days of treatment with amoxicillin, the antibiotic should be replaced with augmentin (0.625 g orally 3 times or 1.0 g 2 times a day) or cefaclor cefuroxime (axetil) (0.5 g orally 2 times a day). In case of allergy to r-lactam antibiotics, modern macrolides are prescribed (rulid 0.15 orally, 2 times a day; spiramycin, 1.5 million IU orally, 2 times a day).
For anesthesia, topical eardrops are used containing equally divided 70 ° alcohol and glycerin; of the patented drugs the same effect has otipax, which consists of 96 ° alcohol, glycerin, lidocaine, phenazone. This composition has an analgesic and anti-inflammatory effect.
With severe earache, endoaural meto-impingal blockade is effective. 1 ml of a 2% novocaine solution and 0.5 ml of subperiosteal hydrocortisone are injected into the posterior wall of the external auditory canal at the border of the cartilaginous and bone sections. Properly performed blockade is accompanied by “whitening” of the skin of the bony part of the auditory canal and eardrum.
Of the systemic analgesics and anti-inflammatory drugs prescribed: paracetamol (tab. 500 mg); diclofenac (tab. 50 - 100 mg, amp. 75 mg / 3 ml); Ketorolac (ketanov) (tab. 10 mg, amp. 30 mg / 1 ml); tramadol (tramal) (tab. 150 mg, capsules 50 mg, suppositories 0.1 g, rr for injection 5% 2 ml).
In the treatment of acute purulent otitis media in order to restore the function of the auditory tube, its catheterization is used. Blowing the auditory tube in acute otitis media using a catheter allows you to drain the middle ear, eliminate the always occurring in this disease air depression in the tympanic cavity, and also introduce medication into it. In addition, catheterization has a beneficial effect on the course of inflammation. The fear of introducing an infection from the pharyngeal cavity into the middle ear is unreasonable, since in acute purulent otitis media the pharyngeal microflora has already penetrated into the middle ear, and the auditory tube has largely lost its protective function.
Catheterization is carried out from the very beginning of the disease, and this often allows for an abortive course of the process; in II - III stages of acute inflammation of the middle ear, blowing with a catheter also gives a good therapeutic effect. Most often after blowing a mixture of dexamethasone solution and antibiotic dissolved in an isotonic solution of sodium chloride is injected into the tympanic cavity through the catheter.
In addition to the main treatment, from the very beginning it is desirable for the patient to prescribe immuno-corrective drugs. In some cases, good results are obtained from the use of physiotherapy.
If, despite the treatment, the patient's condition does not improve, severe pain in the ear continues, persists heat, when pressing on the mastoid process, soreness is pronounced, and when otoscopy the protrusion of the eardrum is observed, then a paracentesis is shown - a section of the eardrum.
Paracentesis is definitely indicated and should be performed according to emergency indications if:
There are signs of irritation of the meninges; the process extends to the inner ear (which may indicate dizziness, nausea and vomiting, ataxia, spontaneous nystagmus); paresis or paralysis of the facial nerve occurs; develops periostitis mastoid.
In young children, paracentesis is used not only for medical purposes, but also for diagnostic purposes. The procedure is also indicated for persons with severe comorbidities. internal organs, the elderly, and if the patient has signs of reduced immune protection.
Paracentesis is performed under local anesthesia, in very restless children, light anesthesia is sometimes used with nitrous oxide. Local application anesthesia is carried out by introducing a wick wick soaked in a 10% lidocaine solution for 10 minutes into the external auditory canal until the eardrum is in contact with the eardrum. However, it is more reliable to carry out infiltration anesthesia subcutaneously into the posterior wall of the auditory canal at the border of the web-cartilage department in the bone.
An incision using a special paracentesal needle is usually performed in the back of the lower quadrant of the eardrum (usually the place of greatest protrusion) from bottom to top through its entire thickness. The depth of insertion of the paracentesis needle is 1-1.5 mm; with a deeper injection, the labyrinth wall can be injured. The incision should not reach annulus tympanicus, so that later resistant perforation is not formed. Usually, the perforation artificially formed during paracentesis closes independently after several days, and all three of its layers coalesce. After perforation with pus, the perforation closes worse, since its edges do not fully stick together and it gapes. After the paracentesis, sterile gauze turunda or cotton wool is inserted into the external auditory meatus. Turunda should be changed frequently, while cleaning the ear canal from pus.
Treatment in the perforated stage. In this stage of acute purulent otitis media, the patient continues to receive antibiotics and antihistamines, and vasoconstrictive nasal drops are still being poured into him to restore the function of the auditory tube. In case of thick purulent discharge, mucolytics are prescribed (fluimucil, ACC, fluifort, synupret; fluditec, carbocysteine-based muco-regulating drug, which affects the quality of the secretion (decreases its viscosity) and regulates its amount (does not increase the secretion), as well as improves the evacuation of the secretion from the tympanic cavity and contributing to more rapid restoration of hearing) and Erespan - an anti-inflammatory drug that reduces hypersecretion and edema of the mucous membrane and stimulates the function of the ciliated epithelium of the auditory tube s. Physiotherapy procedures (UV, UHF or microwave therapy, laser therapy) and warming ear compresses at home also give a good result.
In the presence of perforation of the tympanic membrane, drugs are injected into the middle ear with the help of transtimpanal pressure. The above mixture of antibiotic and dexamethasone (and subsequently, enzymes that prevent the formation of scars in the tympanic cavity — trypsin, himopsin, lidaza, etc.) is poured into the external auditory meatus in the amount of 1 ml and is injected into the external opening of the auditory canal passage. In this case, the medicinal substance passes through the tympanic cavity, the auditory tube and can get into the cavity of the nose and mouth. Catheterization and transtimpanal discharge medicinal substances are effective methods treatment.
Local treatment in this stage of the disease is aimed at providing favorable conditions for the outflow of purulent discharge from the tympanic cavity. In order for the patient to remove the purulent secretion from the depth of the external auditory canal 2–3 times a day, he must be instructed accordingly. The manipulation is carried out as follows: a piece of sterile cotton wool is wound on a probe with cutting or on the free end of a match. Adults are pulled back and up (the child is back and down) and a probe or a match with cotton is gently inserted into the depth of the ear canal to the eardrum. For thick pus, a warm 3% hydrogen peroxide solution is pre-poured into the ear canal. So repeat until the cotton wool does not remain dry.
After removal of purulent secretion, a medicinal solution preheated to 37 ° C is poured into the ear. This may be a 0.5-1% solution of dioxidine, a 20% solution of sodium sulfacyl, otof drops containing the active substance rifamycin, and others. It is not recommended to prescribe alcohol drops in the second stage of otitis because alcohol often causes irritation of the mucous membrane shell drum cavity.
In addition to the main treatment, the patient is usually prescribed immuno-corrective drugs and fortifying agents.
Treatment in the reparative stage. In the final, reparative stage, suppuration stops, the perforation of the eardrum often closes with a tender, inconspicuous scar.
During this period, it is important to achieve the fullest possible hearing recovery. Antibiotic therapy is canceled, the ear toilet and thermal procedures are stopped. The focus is on the restoration of the ventilation function of the auditory tube and the increase in body resistance. They carry out the blowing of the auditory tube along Politzer or through a catheter, perform pneumomassage of the eardrum using a Sigle pneumatic funnel, designate endaural ionophoresis with lidaza. To get away with the restoration of hearing, conduct audiometry control.
The following outcomes of acute purulent otitis media are possible.
Recovery with the restoration of normal otoscopic picture and auditory function. . Transition of the disease to the chronic form (chronic suppurative otitis media) with the formation of resistant perforation of the eardrum, recurrent suppuration and progressive hearing loss. . The development of one of the complications of acute purulent otitis media: mastoiditis (in children - anthritis), petrositis, labyrinthitis, paresis of the facial nerve, intracranial complication (meningitis, abscess of the brain or cerebellum, thrombosis of sigmoid sinus, sepsis, etc.). . The formation of adhesive otitis media - the formation of adhesions and adhesions in the tympanic cavity and between the auditory ossicles, their stiffness and, as a result, progressive hearing loss.
Ear pain in children
Earache is common in children of any age. There is a predisposition to such diseases.
In some children, the pain may occur in the cold. It passes a few minutes after the child enters a warm room.
Wear a hat for your child. It is not necessary to lay cotton wool in your ears.
In general, one should not plug the child’s ears for anything. It does not help to remove sulfur from them, but may cause external otitis (otitis externa) or damage the eardrum. Some cotton wool may remain in the child’s ear, as it is difficult to remove. In the ear passages blocked with cotton, more sulfur is produced.
Infectious ear inflammation is more common in children over 8 years old. Usually the middle ear inflames - that part of it, which is located behind the eardrum. Disease is often preceded by a cold. Inflammation is usually accompanied by fever and vomiting. Children complain of earache and hearing loss. In infants, the temperature rises, they become whiny.
During inflammation, fluid and pus accumulate in the middle ear. Sometimes this leads to rupture of the eardrum, a hole appears in it (perforation), after a while liquid is released. Often, the pain immediately disappears as pressure on the eardrum decreases, causing pain.
Inflammation of the middle ear is usually treated with antibiotics, although there is another opinion on this issue. Some experts believe that ear pain can go away without treatment, although antibiotics contribute to faster recovery. Paracetamol reduces pain and temperature.
Sometimes, after inflammation in the middle ear, fluid remains. Antibiotics help in this case, unfortunately, not always. Therefore, you should contact your doctor 6-8 weeks after recovery to make sure that there is no fluid in the ear. Perforations usually heal by themselves, however it is necessary to check the condition of the eardrum from time to time. Fluid left in the middle ear can cause deafness.
Infectious inflammation of the ear canal, a short tube that connects the eardrum to the external environment, is less common, but can cause severe pain. It is called external otitis (otitis externa), which does not always appear under the action of microbes. Sometimes this inflammation is a form of dermatitis. In such cases, the pain in the ear is not accompanied by fever and other symptoms characteristic of middle ear inflammation. If there is a discharge, then you need to consult a doctor.
Some children have a particular susceptibility to otitis externa and can tolerate this disease several times. Sometimes you yourself can determine the cause of the disease, for example, if you know that a child in the pool or while bathing got water in the ear.
The treatment is as follows: the medicine prescribed by the doctor is instilled in the ears. In some cases, careful removal of dead cells, pus and other contents of the ear canals is necessary. This procedure is also performed by a doctor.
Despite pain, inflammation of the external ear, unlike inflammation of the middle, does not lead to hearing impairment.
Quite often, ear pain causes sore throat and toothache. In such cases, doctors talk about reflected pain that occurs in one place and is felt in another. A sore throat or a bad tooth can cause an earache, even if there is no sore throat or toothache.
Reflected pain in the ears, as a rule, is volatile. Sometimes there is no certainty that the cause of the disease lies outside the ear. In this case, you should also consult a doctor.
Boils in the ears are sometimes very painful. As a rule, the cause of the pain in this case is obvious, although it is sometimes difficult to determine the position of the boil in the ear canal.
The foreign body in the ear can also cause pain and discharge from the ear.
Contrary to popular belief that earwax contributes to earache, this is extremely rare. In fact, earwax practically does not cause any pain in children, although it is the most common cause of hearing impairment. Occasionally, pain causes a hard piece of sulfur to block the ear canal.
Trauma to the ear can be accompanied by pain, especially when the tissues surrounding the ear are bruised. A direct blow to the ear with a flat object, such as a palm, can even cause a rupture of the eardrum. If your child has a bruised ear, complains of tinnitus or hearing loss that lasts more than 5 minutes after the injury, you should consult a doctor.
Pain in the ear with compartments may indicate inflammation of the middle ear with perforation or a foreign body in the ear.
Discharges from the ear that are not compatible with pain may also be caused by some of the reasons mentioned above, but in some cases you may see semi-fluid, brown or black fragments (particles) earwaxwhich are naturally removed from the ear canal. This is perfectly normal, although you should consult a doctor to rule out another disease.
As a rule, you should consult a doctor in all cases if the child complains of earache lasting more than 20 minutes, as well as in the presence of discharge.
Acute otitis media (CCA) in children
Inflammation of the middle ear is one of the common diseases of childhood. According to G.L. Balyasinskaya:
Acute otitis media is 65–70% of all diseases in childhood; peak incidence occurs at the age of 6-18 months; 44% of children carry CCA in the first year of life 1-2 times; 7 - 8% - 3 - 4 times.
The structure of the ear of a newborn child is quite different from the structure of the ear of an adult person. In infants and children of the first years of life there are a number of anatomical and physiological features that determine the originality of the course of otitis at this age.
We list the following:
A relatively short and wide auditory tube through which not only an infection from the nose and nasopharynx, but also food masses when regurgitating can enter the tympanic cavity; the possibility of the amniotic fluid entering the tympanic cavity through the auditory tube during labor, which can provoke inflammation in the middle ear of the child; in the tympanic cavity of a child of the first year of life, remains of embryonic myxoid tissue, which is a nutrient medium for the development of infection, remain; the predominantly horizontal position of infants contributes to venous stasis in the posterior parts of the nose, and this may also play an important role in the occurrence of otitis media; imperfect immune system and thermoregulation of the child; in children of the first years of life, adenoids, occluding the pharyngeal mouth of the auditory tube and being the source of infection, are often the cause of recurrent otitis media. Adenoiditis often goes to the auditory tube and then to other parts of the middle ear, which is facilitated by the functional uniformity of the mucous membrane lining the nasal cavity, nasopharynx, and middle ear. Acute otitis media in newborns and children of the first two years of life is distinguished by a number of pathogenesis, clinical, and diagnostic features.
Undoubted role in the occurrence of otitis media in children early age play prematurity, the pathological course of pregnancy and childbirth, obstetric trauma, artificial feeding. Otitis is more common in children who are malnourished, have avitaminosis, rickets, diathesis. In the occurrence of otitis media at this age, an important role belongs to infectious diseases - measles, scarlet fever, influenza.
Clinic. Manifestations of acute otitis media in infants are characterized by mild local symptoms. They have practically no data from anamnesis, which is an important tool in the diagnosis of older children and adults.
Pain in young patients is manifested by excitement, anxiety, poor sleep, pendulum-like head movements are observed. The child refuses to take the breast because painful swallowingrubs his sick ear on his mother's hand. The temperature is first low-grade, after 1 to 2 days it can rise to 39.5 —40 ° C. An important symptom is soreness when pressing on the trestle, due to the absence of the bony part of the ear canal and the transfer of pressure directly to the inflamed eardrum.
Vascular connections between the middle ear and the cranial cavity, as well as the stony-scaly slit in children of the first years of life, cause symptoms of irritation of the meninges, defined as meningism: convulsions, vomiting, drooping of the head, sometimes blackout. This condition, in contrast to meningitis, does not develop due to inflammation of the meninges, but due to their irritation with bacterial toxins.
Diagnostics. Of great importance is the correct interpretation of the otoscopic picture. The slit-like shape of the auditory canal, the accumulation of epidermis flakes in it, the almost horizontal location of the eardrum — all this makes examination much more difficult. In addition, in infants, the eardrum is thicker, muddy and reddens easily after cleaning the ear and when the baby cries. Spilled hyperemia and infiltration of the eardrum in the absence of its distinct contours are signs of acute inflammation, and in the presence of other clinical manifestations, an acute purulent process and require urgent paracentesis.
Acute otitis media in children goes through the same stages as adults. However, in children more often than in adults, cure can occur without perforation of the eardrum. This is due to its greater resistance, high absorption capacity of the mucous membrane of the tympanic cavity and easier outflow of pus through a wide and short auditory tube.
Treatment. In the complex of therapeutic measures for young children, antibacterial therapy occupies an important place. In particular, at the age of up to 2 years, acute purulent otitis media is an absolute indication for prescribing antibiotics, especially when there are marked clinical signs of the disease and when the temperature rises to 38 ° C and above. Children in more early termsrather than adults, paracentesis is indicated. The indications for paracentesis in each individual case are set individually. In doubtful cases, when the otoscopic picture is unconvincing, and the effects of toxicosis increase, it is better to perform a paracentesis. As with adults, the incision is made in the back quadrants of the eardrum.
In children aged 1 to 3 or 4 years, recurrent acute otitis media is sometimes observed, characterized by repeated inflammatory processes in the middle ear with a frequency of 2-5 to 12-15 times a year. Relapses are associated with the imperfections of the child’s immune system and the disorder of the protective mechanisms of the middle ear in pathology gastrointestinal tract, exudative diathesis, food and drug allergies, pathology of the pharyngeal lymphoid ring, nose and paranasal sinuses.
In case of recurrent otitis media, complex treatment is carried out. In addition to the traditional local and general therapy of the purulent process, during exacerbations, the rehabilitation of the pharyngeal lymphoid ring, the treatment of diseases of the nose and the paranasal sinuses, the normalization of the baby’s nutrition, and the increase in the body’s reactivity are necessary.
Acute otitis media with infectious diseases
Acute inflammation the middle ear accompanying any infectious disease is characterized by a more severe course. It may be etiologically associated with the causative agent of the infection itself; in addition, the resistance of the organism is reduced under the influence of an infectious disease. In infectious diseases, the simultaneous damage of both ears, including all elements of the middle and sometimes the inner ear, and the rapid development of a process that is often necrotic, is often noted.
Typically, flu otitis media can be observed during an outbreak of influenza, often at the beginning. Inflammation of the middle ear can occur in the early period of infection, and then the process has all the characteristics of the underlying disease. Secondary otitis media develops in late period infectious disease.
Flu otitis is characterized by hemorrhagic form of inflammation with the appearance of extravasation (hemorrhage) under the epidermis of the skin of the external auditory canal in the bone region and on the eardrum in the form of hemorrhagic or serous bubbles. Such extravasates are called hemorrhagic blisters, or bullae (hence, bullous otitis). When otoscopy on the background of spilled hyperemia of the eardrum and the skin of the auditory canal, 2 - 3 characteristic rounded hemorrhagic red-purple vesicles are seen, at the opening of which there appears a scant serous discharge.
The inflammatory process in influenza otitis is localized predominantly in the over-drum space and proceeds hard, sometimes with damage to the inner ear and the development of an intracranial complication, meningitis. Medical tactics in this case involves the holding of paracentesis and the implementation of reliable drainage of the tympanic cavity, as well as the appointment of massive doses of antibiotics and drugs that facilitate the patient's condition.
Along with conductive deafness in otitis influenza in some cases, neurosensory damage is detected, requiring appropriate pathogenetic therapy.
Otitis with scarlet fever and measles is characterized by the possibility of developing bone and soft tissue necrotic lesions of the middle ear, which is more common in young children. Necrotizing otitis media for scarlet fever and measles usually develops in the initial stage of the disease, while necrotic lesions are often localized in the pharynx and nose. In measles, otitis begins or precedes the rash.
At the basis of the pathogenesis of necrotic otitis is the development of thrombosis in the vessels of the middle ear, which causes necrosis of the mucous membrane of the tympanic cavity, the auditory ossicles and the bone tissue of the mastoid process.
For measles and scarlet otitis media is characterized by a clinically unexpressed onset, which is masked by the underlying disease. The process in the ear develops unnoticed, pain syndrome is often absent, which can be explained by the rapid necrotic destruction of the eardrum.
The first sign of the disease is often the appearance of heavy purulent discharge from the ear with a sharp putrid odor due to the involvement of the bone in the process. When otoscopy visible extensive perforation of the eardrum, until its complete destruction. The process develops very rapidly, often perforation is formed within one day. The disease most often goes into the chronic stage.
When the necrotic process spreads to the inner ear, a serous or purulent labyrinthitis develops, sometimes with complete deactivation of the auditory and vestibular functions. With bilateral lesion of the labyrinth in young children develop deaf-mutism.
The treatment is directed against the underlying disease and its local manifestations. The timely and adequate use of antibiotics for measles and scarlet fever can dramatically reduce the likelihood of developing necrotic otitis and its inherent complications.
The indication for surgical intervention is the development of necrosis of the mastoid process; the purpose of the operation is the removal of necrotic tissue and drainage of the middle ear cavities.
Complications of acute otitis media
Mastoiditis
it purulent inflammation the mucous membrane and bone tissue of the mastoid process of the temporal bone, the most common complication of acute otitis media. Changes in the mastoid process of mastoiditis vary depending on the stage of the disease. There are two main stages of mastoiditis - exudative and alterative (destructive).
AT exudative stage the mucous membrane and the periosteum of the mastoid cells are involved in the process; at this time, the cells are filled with exudate, and the mucous membrane is inflamed and sharply thickened.
The interactive stage is characterized by the predominance of proliferative-alterative changes, which also extend to the bone structures of the mastoid process. When this occurs, bone destruction by osteoclasts, the formation of granulations. Necrosis of bone bridges develops between the cells, and they merge to form one common cavity filled with pus, and the mastoid empyema is formed.
Mastoiditis is more often observed in patients with the pneumatic type of the structure of the mastoid process. A number of factors contribute to its development: high virulence of the pathogen, decrease in body resistance (in particular, in diabetes, nephritis, other chronic diseases), difficulty in outflow from the antrum and the tympanic cavity. One of the reasons for the development of mastoiditis is irrational treatment of acute otitis media.
The process of bone destruction in the alteration stage can reach the dura mater of the middle or posterior cranial fossa and cause various intracranial complications. Pus can burst to the surface of the mastoid process (with the formation of a subperiosteal abscess), to the zygomatic process or to the scales of the temporal bone, to the stony part of the pyramid of the temporal bone, through the apex of the process to the interfascial spaces of the neck.
The causative agents of mastoiditis are the same microorganisms that cause the development of acute suppurative otitis media.
The clinical picture of the disease is characterized by general and local symptoms.
Common symptoms — a worsening of the general condition, an increase in body temperature, a change in the composition of the blood — do not significantly differ from the manifestations of acute purulent otitis media. Diagnostic importance is the analysis of the dynamics of these signs in case of suspected possible involvement in the inflammatory process of the mastoid process.
Usually it takes 2 - 3 weeks from the onset of acute otitis media and against the background of improving the clinical picture, the general condition worsens again, the temperature rises, pain and suppuration from the ear resume. However, it must be remembered that suppuration may be absent if the outflow of pus from the middle ear is impaired (“aditus block”).
The pain is often localized in the ear and in the region of the mastoid process; in some patients it covers half of the head on the side of the lesion and increases at night. On palpation and percussion of the mastoid process, pain is noted, often in the apex or area of the mastoid process. There are also complaints of noise in the ear or head on the side of the patient's ear and pronounced hearing loss.
Examination of the patient sometimes reveals hyperemia and infiltration of the skin of the mastoid process, which is a consequence of periostitis. You can also observe the smoothness of the ear crease and protrusion of the auricle anteriorly.
Suppuration from the ear is often profuse, having a pulsating character - pus-like pus fills the external auditory canal immediately after cleaning
ear. Sometimes the usual suppuration through the perforation in the eardrum joins heavy discharge pus through the back wall of the external auditory canal. To establish the cause of such an increase in suppuration is possible only with a thorough cleaning of the ear and the detection of a fistula, from which pus is released.
Such a variant of the flow of mastoiditis is also possible, in which there is no otorno. This happens in violation of the outflow of pus, if the defect of the eardrum was closed or formed a block entrance to the cave.
Diagnostics. An important otoscopic sign of mastoiditis is the winding of the posterior surface of the external auditory canal in the bone region. The overhang is associated with the development of periostitis and the pressure of the pathological contents in the area of the anterior wall and the cave entrance. In the same place, a fistula sometimes forms, through which pus enters the external auditory canal. Mastoiditis eardrum is often hyperemic, infiltrated.
In the diagnosis of mastoiditis, radiography of the temporal bones in the projection by Schuller is of great importance. With mastoiditis on the radiograph, one can see a decrease in the intensity of pneumatisation, the veiling of the antrum and mastoid cells. In the later stages of the process, with the destructive form of mastoiditis, one can see the destruction of the bone septums and the formation of areas of enlightenment due to the formation of cavities, made with pus and granulations.
The spread of the process in the mastoid process and its transition to adjacent anatomical structures depends on the development of air cells in different parts of the temporal bone - in the scales, zygoma, pyramid, etc. Inflammation in these places is sometimes accompanied by a breakthrough of pus into the surrounding soft tissue.
The breakthrough of pus through the cortical layer onto the outer surface of the mastoid process leads to the formation of a subperiostal abscess. Anterior to his swelling and pastos skin ear area, the smoothness of the ear crease and protrusion of the auricle are enhanced.
Atypical forms of mastoiditis
The spread of pus from the apical cells of the mastoid process to the interfascial spaces of the neck is referred to as apical cervical mastoiditis. Its various forms, named after the authors, differ in the place of pus breakthrough in the apex of the mastoid process.
Betsold's mastoiditis (cervico-apical) is characterized by pus breakthrough through the inner surface of the mastoid apex under the sternoclavicular mastoid muscle with spreading to the neck. It is often observed dense swelling of the soft tissues of the neck - from the apex of the mastoid process to the clavicle.
Orleans' mastoiditis is characterized by the breakthrough of pus through the inner wall of the apex of the mastoid process into the fascial sheath of the spermus muscle.
At the same time, a fluctuating infiltrate develops around the site of attachment of the muscle.
Moura's mastoiditis (neck-jugular) - with this form, pus erupts through the incisura digastrica, spreads under the digastric muscle and penetrates into the para-pharyngeal space with the formation of a deep abscess of the neck.
If the pus from the perisinusal abscess penetrates under the soft tissues of the neck and neck, the process is referred to as cervico-occipital mastoiditis Chitelly.
The spread of a purulent-destructive process on the base of the zygomatic process is called zygomaticitis, and on the scales of the temporal bone, squamite.
It is also possible the spread of pus from the mastoid process through the cellular system into the pyramid of the temporal bone. In this case, petrositis develops, the clinical picture of which is called the Gradenigo triad and includes acute otitis media with suppuration from the ear on the affected side; trigeminitis with pain in the depth of the head, behind the eye; paresis or paralysis of the abducent nerve.
Atypical forms of mastoiditis are the most dangerous, as they often cause various complications. Their occurrence and course are associated with such factors as the age of the patient, the general and local reactivity of his body, the structure of the temporal bone (in particular, its cellular structure), the virulence of the pathogen.
With an atypical course of the process, there is no pronounced sequence of stages of development of inflammation, some symptoms do not have a characteristic clarity. So, the pain either does not bother at all, or it is weak. Suppuration may be minimal or absent altogether. At the same time, it should be borne in mind that atypical forms are almost always accompanied by extensive destruction of the bone, and the development of intracranial complications is possible.
Treatment. There are conservative and surgical treatment of mastoiditis. But in any case it should be carried out in the conditions of an ENT hospital as it is necessary to take into account the possibility of the development of severe complications.
The basis of conservative therapy, appropriate active treatment acute otitis media, is antibiotic therapy, during which prescribe drugs wide spectrum actions, with preference given to p-lacgamic antibiotics.
An important component of the treatment of mastoiditis is to ensure the free flow of pus from the middle ear and local use of antibacterial drugs, which must be prescribed taking into account the sensitivity of the ear flora. Conservative treatment is successful in the initial stage of mastoiditis, while bone damage has not yet occurred and the exudate outflow is not disturbed.
If during the conservative treatment the objective symptoms do not change or increase, resort to surgical treatment of mastoiditis. An absolute indication for emergency surgical intervention is the appearance of signs of intracranial complications, the occurrence of complications in the areas bordering the middle ear (subperiosteal abscess, pus outbreak in the apex of the mastoid process, the development of zygomaticitis, squamite, petrositis). The operation is definitely indicated if a patient with mastoiditis developed signs of otogenic paresis or facial nerve paralysis or labyrinthitis developed. In all these cases, an anthromastoidotomy is performed — an opening of the antrum and trepanning of the mastoid process.
The operation is performed under endotracheal anesthesia, adults in some cases operate under local infiltration anesthesia. With a scalpel make an incision in the skin, subcutaneous tissue and periosteum, retreating 0.5 cm from the transitional fold behind the auricle; incision length is 5-6 cm. The soft tissue with the periosteum is separated by the Raspusor, exposing the cortical layer in the area of the mastoid process, after which a lira retractor is applied.
Bone trepanation is performed using bits of various sizes, for this you can also use cutters. Removing the affected bone, gradually deepen towards the cave, which must be necessarily opened to ensure drainage of the tympanic cavity. The cave is located at a depth of 1.5 - 2 cm from the surface of the mastoid process, in the projection of the junction back wall external auditory canal to the top. It can be verified that the opened cavity deep in the bone wound is the cave of the mastoid process by probing with a bell-shaped probe, which through aditus ad antrum easily falls into the tympanic cavity. In addition, at the bottom of the cave one can see the bulging of the ampoule horizontal semicircular canal.
The further course of the operation involves the thorough removal of cariously altered bone, pus and granulations. In the case of an extensive carious process, all cellular groups, including apical, perisinous, zygomatic, perifacial, etc., are sequentially opened. At the end of this stage of the operation, the edges of the bone wound are smoothed with a bone spoon or cutters.
Elimination of a purulent focus in the mastoid process is completed by demolishing the posterior wall of the external auditory canal to the level of the ampulla of the horizontal semicircular canal, however, the annulus tympanicus is retained. The plastics of the posterior skin wall of the auditory meatus are also performed; the flap is hemmed in the lower corner of the wound.
The operation is completed by washing the wound with a warm antiseptic solution, drying, tamponade with turunds soaked in levomekol, and applying a primary suture to the wound in the ear area. The exception is mastoiditis with subperiosteal abscess - the postoperative wound in this case is left open. This is also done in most cases after an extended mastoidotomy in patients with otogenic intracranial complications.
It should be noted that when performing an operation for any form of mastoiditis, one should not limit oneself only to the opening of the cave and the surrounding perianthral cells.
Mandatory surgical revision of the entire cellular system of the mastoid process. Particular attention is paid to the angular and threshold cells, as well as the cells of the apex of the mastoid process.
In the case of mastoiditis, Bezold and Mure, the behind-the-ear incision of the soft tissues is extended to the neck along the anterior edge of the sternocleidomastoid muscle. This allows drainage of pus accumulation in the fascial vagina of the indicated muscle and in the parapharyngeal space.
In the case of mastoiditis, Chatelli's behind-the-ear incision is supplemented with a transverse, directed posterior through the middle of the occipital-cervical infiltrate. After emptying the subperiosteal abscess, an expanded mastoidectomy is performed with an exposure and diagnostic puncture of the sigmoid sinus.
In patients with zygomaticite, the behind-the-ear incision of the soft tissues continues anteriorly and upward, and, bending around the upper attachment of the auricle, expose the base of the zygomatic process of the temporal bone. After a typical mastoidotomy, the cortical layer of the zygoma is removed and, starting from the anterior surface of the exposed antrum, the zygomatic cells with pus and granulations are removed with a sharp spoon.
When spreading the process from the mastoid process to the scales of the temporal bone (squamous), behind-the-ear section
soft tissues extend up to 2–3 cm; after a typical mastoidotomy, the affected bone of the scales is removed with forceps and a sharp spoon.
Antritis
In newborns and infants, the mastoid process is not developed, and the purulent process from the middle ear penetrates only into the antrum. In this case, the inflammatory process in the cave and in the surrounding tissues is designated as antritis.
An important feature of antritis in children is that the formation of subperiosteal abscess occurs fairly quickly, sometimes even without destroying the bone substance; at the same time pus gets through nezabroshy cracks (fissura squamo-mastoidea or fissura tympano-mastoidea).
Clinic. In case of antritis, the child’s reaction to pain is manifested by anxiety - he often cries, does not sleep well at night, his appetite is disturbed; there are often signs of meningism, the temperature can rise to 38 - 39 ° C. In some cases, the pain is absent, the temperature is low-grade or even normal, but the child is sluggish, inhibited.
The ear canal is filled with thick, cream-like pus; having wiped the ear with a cotton swab, it can be cleaned, but very soon the ear canal is again filled with purulent exudate.
Diagnostics. When otoscopy you can see the blurring of the identification points of the eardrum, the change in its color - from dark purple to pink or grayish; sometimes the eardrum protrudes, mainly in the posterior-upper quadrant. Pulsation is visible in the perforation area. Diagnosis of antritis is often difficult due to mild local symptoms. Trial paracentesis, timpano-or anthropuncture can help in the diagnosis.
Anthropuncture is performed in the position of the child "lying on his back", his head is turned in the direction of the healthy ear. After treating the skin behind the auricle with 70%
with alcohol and infiltration anesthesia with a 0.25% solution of novocaine, puncture is performed with a special thick needle, equipped with a depth control regulator. The reference point is the transitional fold behind the auricle, the puncture site is located posteriorly and 2–3 mm above the upper wall of the external auditory canal. Than less child, the higher antrum is located. The needle is inserted in the direction anteriorly and upward to a depth of 0.5 - 1 cm. When it enters the antrum, there is a feeling of falling into the cavity. The contents of the antrum (pus, mucus) are sucked through a needle through a syringe, after which the antibiotic dissolved in an isotonic solution is injected into it. Sometimes a Teflon tube is inserted into the cave through the same needle, which makes it possible to regularly flush the antrum and inject drugs into it.
Treatment. Surgical treatment - anthrotomy - is indicated in the absence of effect from the conservative treatment of anthritis, especially when signs of osteomyelitis appear in the perianthral region. The operation is performed under local anesthesia with a 0.5% solution of novocaine with adrenaline. Very carefully, in layers, behind the auricle they make an arcuate incision of soft tissues 15 mm long. In infants, the cortical layer is very soft and thin, so the separation of soft tissues should be done very carefully. The antrum is projected above and backwards from the posterior surface of the external auditory canal, it is located superficially and is larger than in adults.
After opening the antrum, pus and granulations are removed from it. The postoperative cavity is washed with an antiseptic solution, loosely tamponed with turunda with levosin or antibiotic solution. In the postoperative period, to ensure optimal drainage, the dressing is changed daily. The child is prescribed parenteral antibiotics, fortifying therapy. The cure usually occurs 2 to 3 weeks after surgery.
Middle ear injuries
With middle ear injuries in 90% of patients reveal a rupture of the eardrum. It can occur as a result of a sudden increase or decrease in pressure in the ear canal when hitting the ear, falling on it, playing snowballs, jumping into the water, as a result of an air wave during explosions at close range. Damage to the eardrum can occur when manipulating various objects in the ear (matches, hairpins, etc.), when a sudden jolt causes the eardrum to rupture. Damage to the eardrum by small branches is possible when walking or running through shrubs. Sometimes unskillful attempt to remove leads to injury foreign body from the auditory canal.
Damage to the eardrum is accompanied by pain in the ear, noise and hearing loss. When otoscopy observed hemorrhages in the eardrum, hematomas in the tympanic cavity, often reveal defects in the eardrum of various shapes and sizes. Perforation can be slit-like, dotted, rounded, sometimes with jagged edges; it can occupy one quadrant or more. More often it is located in the front-bottom quadrant. Through the perforation formed during otoscopy, it is sometimes possible to see the medial wall of the tympanic cavity, the mucous membrane of which in the presence of fresh injury is often hyperemic.
Treatment. The patient and the physician should take maximum care so that through the defect of the eardrum does not introduce the infection into the middle ear. It is necessary to avoid all sorts of manipulations in the ear, the appointment of drops in the ear and its washing is absolutely contraindicated.
First aid should be limited to the introduction into the external auditory meatus of a sterile turunda or cotton ball with boric alcohol for 5 —7 days. To prevent the development of inflammation in the middle ear, antibiotics are prescribed, and measures are taken to preserve the aeration of the tympanic cavity through the auditory tube.
Prevention
Prevention of inflammatory diseases of the middle ear involves the elimination or weakening of the influence of those factors that contribute to the emergence of acute otitis media and its transition to chronic. A significant role in the prevention of inflammatory diseases of the middle ear is played by the timely rehabilitation of chronic foci of infection in the nose and throat, the restoration of normal nasal breathing.
For infants, it is important to have normal breastfeeding, hardening to reduce the incidence of infections such as influenza, measles and scarlet fever.
Prevention of recurrent acute otitis media and its transition to chronic - is primarily proper treatment the patient. An important component of this treatment is a timely performed (if indicated) paracentesis, as well as adequate antibiotic therapy, taking into account the characteristics of the pathogen and its sensitivity to existing drugs. In particular, the transition acute otitis in chronic, it is often conducive to the early cancellation of the antibiotic, its use in small doses and the lengthening of the intervals between administrations of the drug.
Patients who have had acute otitis media, even with a favorable course of the recovery period and with the normalization of the otoscopic picture and hearing, should be under the supervision of a physician for 6 months. By the end of this period, they must be re-examined, and if signs of trouble are found in the ear (slight hearing loss, changes in the otoscopic picture, impaired tubular function), the treatment should be repeated: hold the auditory tube, massage the eardrum, prescribe biostimulants, etc. up to the operation (tympanotomy, shunting of the tympanic cavity).
Chronic suppurative otitis media
Chronic suppurative otitis media (CHD) is characterized by a triad of clinical features:
The presence of resistant perforation of the eardrum; recurring otorrhea; progressive hearing loss.
The combination of these signs allows you to confidently diagnose chronic suppurative otitis media.
However, in some cases, the disease can occur with minimal severity or even the absence of one or two of these symptoms. Perforation of the tympanic membrane can be distinguished only when viewed under a microscope, or even covered with epidermal scales or scar tissue. Suppuration from the ear may be absent for decades. Hearing loss can be subjectively not manifested for a long time, and it can be detected only with careful audiological research, and in some cases the hearing practically corresponds to the age norm. In this case, the pathological process in the middle ear steadily progresses and may lead to the development of serious complications.
Epidemiology. Despite the decline in the incidence of chronic suppurative otitis media, which is associated with timely rehabilitation of the upper respiratory tract and proper treatment of acute otitis, its prevalence in the population remains quite high, ranging from 13.7 to 20.9 cases per 1000 population. Among other diseases of the upper respiratory tract, the treatment of which takes place in the hospital, the frequency of chronic otitis media is 20-25%.
Etiology. Chronic suppurative otitis media is usually the result of acute acute purulent otitis media or rupture of the eardrum in trauma. More than half of cases of illness begin in childhood.
Pseudomonas, Staph, aureus, Proteus, Esherichia coli, Klebsiella pneumoniae are commonly found among the causative agents of HGSO. With a long course of the disease, mushrooms, such as Candida, Aspergillus, and Misog, are increasingly detected. Anaerobic bacteria, which are present in chronic purulent otitis media in 70–90% of patients, also play a significant role, with Bacteroides, Fusobacterium, Peptococcus, Lactobacillus being most commonly found.
The transition of the acute form of otitis media to chronic is associated with the action of a number of adverse factors:
Virulence of the pathogen resistant to the use of antibacterial agents; a decrease in body resistance, which is observed in chronic infections; violation of local and general immune defenses; blood diseases, diabetes, rickets, etc.
A significant role in the development of chronic suppurative otitis media is played by the pathological condition of the upper respiratory tract, for example, the presence of adenoids, curvature of the nasal septum, chronic sinusitishypertrophic rhinitis.
Pathogenesis.Violations of the drainage and ventilation functions of the auditory tube lead to difficulty in evacuating the contents of the tympanic cavity and impairing aeration of the middle ear cavities. This, in turn, prevents the normal healing of perforation of the eardrum after suffering acute purulent otitis media, which leads to the formation of resistant perforation.
In some cases, inflammation of the middle ear from the very beginning acquires the features of a chronic process, for example, with necrotic forms of otitis media, with sluggish otitis media with perforation in the loose part of the eardrum, with tuberculosis, diabetes, in elderly and senile people.
Classification
In accordance with the International Classification of Diseases (ICD-10), by the nature of the pathological process in the middle ear, by the characteristics of the clinical course and the severity of the disease, HGSO is divided into two forms:
Chronic toubioimpanal purulent otitis media - mesotympanitis; chronic epitympano-antral purulent otitis media - epitimpanitis.
These names reflect the presence of purulent-inflammatory changes in the mucous membrane of the auditory tube and the tympanic cavity - in the first case and the involvement in the pathological process of bone tissue of the anticoantral region and the mastoid cells - in the second.
The main clinical difference between these forms is that mesotympanitis is characterized by a relatively favorable course, the perforation of the eardrum in this case is located in the tensioned part of it. For epitimpanita characterized by poor quality severe course, and the perforation is localized in the loose part of the eardrum. Fundamentally important is the fact that only the mucous membrane is involved in the inflammation of the mesotympanitis, and the bone is not affected by caries; with epitimpanity, deeper tissue damage occurs, and the bony structures of the middle ear are involved in the destructive (carious) process.
It is important to note that sometimes patients with perforation localized in the tensioned part of the eardrum can also develop bone destruction (caries) in the deep sections of the middle ear, as a result of which cholesteatoma is formed. This is usually the case when the perforation is marginal, i.e. comes to the bone ring (annulus tympanicus).
In practice, they sometimes distinguish the third form of HGSO - epimesotimpanitis, which is characterized by an extensive, “Subtotal” defect of the eardrum and poor-quality current inherent in epitimpanitis.
HGSO Mesympanic
Chronic purulent mesotympanitis is observed in 55% of patients with chronic purulent otitis media. In the tympanic cavity with this form of the disease often contains mucous or mucopurulent secretion. The mucous membrane of the tympanic cavity itself is thickened, with the conducted histological analysis reveals inflammatory edema, chronic lymphoid plasmocytic infiltration with an admixture of leukocytes and an increase in the number of goblet cells.
Proliferation of the mucous membrane is accompanied by the formation of multiple small true cysts in the submucous layer, as well as the development of granulations or polyps. The auditory ossicles are usually preserved, but in some patients they may be partially destroyed. Cicatricial changes in the chain of the auditory ossicles are more pronounced around the stirrup, as a result of which fixation of the base of the stirrup in the niche of the vestibule may develop.
The aditus block in case of mesotympanitis develops in 15–20% of cases, while anaerobic conditions are created in the cellular system of the mastoid process, contributing to the development of aggressive microflora, which leads to destruction of the mucous membrane and caries of the mastoid bone.
Clinic. Patients complain of hearing loss and intermittent suppuration from the ear. Discharges from the ear are more often odorless and have a mucopurulent character, but in the presence of granulations or polyps one can observe bloody purulent discharges. By volume, the compartment can be scarce, and during an exacerbation it can be plentiful.
When otoscopy visible preserved stretched part of the eardrum and perforation in pars tensa. Perforation may be different in shape, size and location.
Nekraevaya perforation does not reach the bone ring (annulus ty-mpanicus), and around the circumference there is a narrow rim of the remnants of the eardrum, for which this type of perforation is sometimes called the rim. The pathological process in the ear with such a perforation is considered prognostically more favorable.
When the marginal perforation in the stretched part of the eardrum, reaching the bone ring, there are conditions for the epidermis grows into the tympanic cavity, and this creates prerequisites for unfavorable flow of mesotympanic.
The hole in the eardrum can be round, oval, kidney-shaped. In some cases, the edges of perforation can be spliced with the medial wall of the tympanic cavity, and connective tissue strands can capture the auditory ossicles, disrupting their mobility.
In the diagnosis of mesotympanitis, in addition to traditional otoscopy, microtoscopy should be used, which allows a detailed examination of the remnants of the eardrum and visible parts of the tympanic cavity and assess the condition of the mucous membrane of the promontory wall.
Hearing with mesotympanitis is reduced mainly by the conductive type, the degree of hearing loss depends on the location of the perforation, its size and the nature of pathological changes in the tympanic cavity. When perforation in the anterior parts of the eardrum, hearing can be reduced by 15–20 dB or remain within the normal range. With a long course of mesotympanitis and its frequent exacerbations due to intoxication of the inner ear, the neurosensory component of hearing loss is additionally developed.
Epitimpanit
Chronic suppurative epitimpanitis - a form of chronic hepatitis C, in which there is damage to the bony structures of the middle ear. Pathological changes are localized mainly in the suprabarrel space and the mastoid process, the perforation usually occurs in the loose part of the eardrum, but may also extend to its other departments.
Epitimpanit is characterized by more severe, compared with mesotympanic, course. In this form of chronic hepatitis B, along with the morphological changes noted during mesotympanitis, there is also a lesion of the bony structures of the middle ear; As a result, caries develops in the bony walls of the attic, aditus, antrum and mastoid cells. In addition, in epitimpanitis, in most cases cholesteatoma (epidermal formation) is formed, which also causes pronounced destructive changes in the bony structures of the middle ear.
Depending on which pathology prevails, carious lesion of bone tissue or changes caused by the formation of cholesteatoma distinguish between purulent-carious and cholesteatoma forms of epitimpanitis. However, such a division is conditional, since it is often possible to detect both changes in the affected cavities of the middle ear.
When purulent-carious form of the process is localized mainly in the attic - the upper section of the tympanic cavity. Localization of inflammation in the rebar rebar associated with the structural features of this department. There are numerous folds, pockets of the mucous membrane, the infectious process in which it is difficult to conservative treatment. Changes in bone tissue of varying severity are most often located in the region of the lateral wall of the attic and above the entrance to the cave, while the auditory ossicles, which are mainly located in the rebar space, are often affected.
Cholesteatoma form. Cholesteatoma is a tumor-like formation of a whitish color, with a pearly luster, usually having a connective tissue sheath - a matrix covered with a multilayer flat epitheliumtightly attached to the bone and often growing into it. The basis of cholesteatoma is a dense layering of epidermal masses and their decay products, mainly cholesterol, pus, bacteria.
The formation of cholesteatoma is associated with the growth of the epidermis of the skin of the external auditory canal into the cavity of the middle ear, which becomes possible with edge perforation of the eardrum. Under these conditions, there is no obstruction in the form of remnants of the eardrum between the skin of the auditory canal and the drummed space. The epidermis ingrown in this way is the sheath of cholesteatoma - its matrix.
The matrix is a live formation: its epidermal layer is constantly growing and exfoliating (which is a normal process for the skin), and under the influence of irritation with pus and decomposition products, this process only intensifies. Constant desquamation of the surface layers of the epidermis, its delay and accumulation in the narrow cavities of the middle ear - all this is the process of growth of cholesteatoma.
Increasing cholesteate fills the attic and antrum and destroys the surrounding bone - the labyrinth bone capsule, the wall of the facial nerve canal and the mastoid process, resulting in an exposure of the membranes of the temporal lobe of the brain, cerebellum and sigmoid sinus wall. Over time, this process can lead to severe complicationsincluding intracranial. This pathology contributes to the constant pressure of the mass of cholesteatoma, the ingrowth of the matrix into the bone cells and the empty canaliculi of the bony walls, as well as the effect on the bone tissue of the chemical components of cholesteatoma and its decay products.
Clinic. The main complaint of patients who develop purulent-carious process - discharge from the ear. Discharges are usually purulent, with an unpleasant putrefactive smell, sometimes (in the presence of granulations) with an admixture of blood or "tiny" masses. The sharp unpleasant smell of discharge from the ear is associated with caries of the bony walls, at which purine compounds (indole, skatole) are formed.
When otoscopy in patients with this form of epitimpanitis in the initial stage of the disease, you can see a small perforation in the relaxed part of the eardrum. Increasing gradually, the perforation completely occupies the lateral wall of the attic, the loose part of the eardrum and the bony part of the wall, often with a transition to the posterior-upper wall of the external auditory canal. Granulations can be seen through the hole formed, and when probing the bone edge of the perforation, a roughness is felt.
In patients with epitimpanitis, a more pronounced decrease in hearing is observed than with mesotympanitis. Caries extends to the auditory ossicles, and the joint between the anvil and malleus is often destroyed. In addition, the sound-perceiving apparatus is damaged, which is associated with intoxication of the inner ear through the secondary membrane of the cochlea window and the annular ligament of the vestibule window.
Cholesteatoma epitimpanitis form can occur for a long time without pronounced clinical manifestations. The formation and growth of cholesteatoma occur without pain sensations. The patient notes only periodic suppuration from the ear and hearing loss, to which (especially in a one-sided process) he becomes accustomed and therefore may not pay attention to the existing symptoms for a long time. But although outwardly the cholesteatoma epitimpanitis has been proceeding relatively calmly and imperceptibly for years, the destruction of the bony walls of the middle ear has been steadily progressing. The probability of the development of severe complications, including life-threatening ones, with this form of epitimpanitis is very high.
For uncomplicated purulent-carious or cholesteatom epitimpanitis symptoms such as ear pain, headache, dizziness, unsteadiness of gait are not characteristic. Their appearance indicates an emerging or already existing complication. Pain can be the result of intoxication of the meninges when there is difficulty in the outflow of pus caused by granulations, polyps, swollen cholesteatomas masses. Vertigo and unsteady gait may be associated with the formation of a fistula in the labyrinth capsule, usually it occurs in the area of the ampulla of the horizontal semicircular canal. The destruction of the bone wall of the fallopian canal leads to the development of paresis of the facial nerve.
The appearance of the above complaints in a patient with chronic purulent epitimpanitis is the reason for his urgent hospitalization in the ENT hospital for examination and surgical treatment.
In practice, sometimes the diagnosis of "epimesotoim panit" occurs. This term usually designates a mixed form of the disease, in which a subtotal or total eardrum defect is additionally detected in a patient with chronic purulent otitis media. In this case, all parts of the tympanic cavity are affected by the process, cholesteatoma, granulation, signs of bone destruction often develop. The approach to the management of such patients is the same as with epitimpanitis.
Diagnostics
The diagnosis of HGSO is usually made based on anamnesis, clinical manifestations and an otoscopic picture.
Distinctive features of mesotympanic are:
The presence of persistent non-perforation in the pars tensa - the stretched part of the eardrum; mucous, mucopurulent or (rarely) purely purulent discharge without odor; hearing loss is mainly conductive; the absence of destructive changes on the radiograph and CT of the temporal bone.
The appearance of the smell of purulent discharge indicates the involvement of bone in the carious process, which indicates the transition of the disease into a poor-quality form. With an extensive defect of the tympanic membrane, it is possible to penetrate the attic with a bellied probe and feel its walls: with a mesotympanitis, they are smooth, and there will be no rough sensations indicating caries.
The diagnosis of epitimpanitis is already evident when perforation is detected in the loose part of the eardrum. Violation of the integrity of the eardrum can spread to the bony lateral wall of the attic, often to the posterior surface of the external auditory canal. When probing the bone edge of the perforation, there is a roughness.
In some cases, the defect of the eardrum is very small, located in the epitimpanal part of the membrane or in the depth of its funnel-shaped retraction, and sometimes it can be covered with a purulent crust. It is possible to detect such perforation only with otomicroscopy, the implementation of which is recommended in all cases, especially in doubtful cases.
Additionally, this diagnosis is confirmed by the following symptoms:
Unpleasant putrid odor of purulent discharge (sometimes in the pus is an admixture of blood or "tiny" masses); pronounced hearing loss of a mixed type; presence of bone-destructive changes on radiographs and CT of the temporal bone.
The pattern of epitimpanitus does not depend on the size of the perforation, often with its microscopic dimensions in the bony structures of the middle ear reveal pronounced destructive changes.
Recognizing cholesteatoma is not difficult if typical white (mother-of-pearl) cholesteatoma masses are visible in the perforation lumen.
In other cases, cholesteatoma can be recognized by washing the drumhead through the ear cannula. Detection of floating epidermal flakes in the washing liquid indicates the presence of cholesteatoma.
When probing through perforation using a curved bell-shaped probe, a roughness is detected along the edge of the lateral wall of the attic, and cholesteatomic masses often stick to the tip of the probe.
When cholesteatoma in the bone section of the external auditory canal often occurs overhang of the posterior-upper wall, which is accompanied by a narrowing of its deep sections. This symptom indicates the spread of cholesteatoma under the periosteum of the external auditory canal.
An important method of research in various forms of chronic hepatitis C is the radiography of the temporal bones in the projections of Schüller and Meier, which allows to assess the state of the cellular system of the mastoid process and the attico-antral region. With a long course of the disease, the sclerotic structure of the temporal bone can be seen on the X-ray of the patient's ear.
The underdevelopment of the temporal bone (“infantile” temporal bone) found on the roentgenogram suggests that chronic suppurative otitis media occurred in a patient in childhood. And in some cases, as a result of X-ray examination, even with a successful otoscopic picture, the destruction of the temporal bone can be detected, which is manifested by abdominal formations, signs of sequestration, and destruction of the bone in the atticoantral region.
With a cholesteatoma on the radiograph, a sharply defined bone defect in the attico-antral region is noticeable. It has the appearance of an unstructured enlightenment (cavity) surrounded by a thin dense bone - the cavity wall. In a carious process in the bone, the edges of the defect are usually blurred.
Currently, computerized tomography (CT) of the temporal bones has acquired great importance. It allows you to diagnose cholesteatoma, defects of the auditory ossicles, soft tissue formations (granulations, polyps) in the tympanic cavity and the cellular system of the mastoid process, bone destruction in the roof area of the antrum, the tympanic cavity and the bone wall of the sigmoid sinus, the fact that the process has spread to the skull cavity.
Treatment
Currently, the basis of treatment in all forms of chronic hepatitis C is surgical intervention as soon as possible. The sooner it is produced, the greater the chances of a complete cure for otitis media and the restoration (preservation) of auditory function.
Conservative treatment of a patient with chronic hepatitis C is advisable only as a preparation of the patient for surgery and should be carried out within 1-3 months before the operation. As an independent method of treatment, it can be used only in the event of the patient refusing the operation or the impossibility of carrying it out due to the severe physical condition of the patient.
Conservative treatment
Conservative treatment can be local and general.
Local treatment begins with a careful toilet of the tympanic cavity. It is advisable to carry out its washing with aqueous isotonic antiseptic solutions (furatsilina, 0.5% dioxidine solution, 2% hydrogen peroxide solution). The improvement of the evacuation of pathological contents is facilitated by the use of proteolytic enzymes (trypsin, chymotrypsin, lidz) and mucolytics (acetylcysteine, fluimucil, sinupret).
The penetration of drugs into various parts of the tympanic cavity is facilitated by the trans-impanal injection of medicinal substances. To reduce swelling of the mucous membrane of the middle ear cavities and better penetration of antibacterial, anti-inflammatory and other drugs into them, it is better to start injection with vasoconstrictor agents (adrenaline, galazolin, vibrocil).
Polyps or granulations covering the perforations should be removed (possible on an outpatient basis).
In the presence of cholesteatoma in the cavities of the middle ear, washing with antiseptic aqueous solutions can cause it to swell and lead to worsening of the outflow of the pathological secretion. Therefore, if cholesteatoma is suspected, the washing of the tympanic cavity should be carried out with alcohol-containing solutions, for example, with a 3% alcohol solution. boric acid.
Local or system antibacterial drugs can only be entered based on the results of the antibiogram. Before obtaining the results of microbiological research, broad-spectrum antibiotics are used, taking into account the possibility of participation in the inflammatory process of aerobic-anaerobic associations of microorganisms and fungi. It is advisable to use a combination of antibiotics such as cephalosporins, rifampicin, chloramphenicol, metronidazole with the treatment of the walls of the auditory canal with nitrofungin.
Steroid hormones (hydrocortisone, prednisone, dexamethasone) reduce the swelling of the mucous membrane, reduce the activity of exudative and proliferative processes, contribute to the restoration of the normal cellular composition of the mucous membrane. However, it should be borne in mind that with prolonged use of corticosteroids can stimulate the growth of fungal flora.
Local drug treatment during exacerbation, it should be supplemented with physiotherapeutic methods: ultraviolet irradiation, laser therapy with low-energy helium-neon laser, irrigation of the tympanic cavity with oxygen.
To restore the drainage and ventilation functions of the auditory tube, vasoconstrictor, antibacterial, and hormonal preparations are introduced into it trans-impantially and through the catheter; perform blowing of the auditory tube, electrical stimulation of the muscles of the pharynx, laser therapy of the pharyngeal and tympanic mouths of the auditory tube.
The general conservative treatment methods include the prescription of fortifying drugs, immunomodulators and hyposensitizing agents. It should also be remembered about the need to normalize nasal breathing, both conservative and surgical methods, sanation of inflammation in the nasal cavity and near-nasal sinuses, nasopharynx, oropharynx.
Surgery
Surgical treatment of chronic hepatitis C is aimed at both the rehabilitation of the inflammatory focus and the prevention of intracranial complications, and the improvement or preservation of hearing. Exacerbation of chronic suppurative otitis media should be regarded as a condition that can lead to the development of otogenic intracranial complication. Such patients are urgent, they are urgently sent to the hospital, where, if necessary, the operation is performed urgently.
As already mentioned, the surgical method is fundamental in the treatment of chronic hepatitis C, however, radicalism in operations on the middle ear in our day is gradually being superseded by sparing sanitizing intervention with simultaneous implementation of hearing-improving elements (in some cases they are performed at the second stage of the operation).
The choice of methods of operation is individual and depends on the duration of HGSO, the degree of prevalence and severity of the pathological process, anatomical features mastoid process, the degree of auditory disorders, the state of the auditory tuba, intracranial and labyrinth complications, the qualifications of the surgeon and the availability of modern equipment.
They use various modifications of operations, both sanitizing rumors and rumors. Depending on the state of the auditory tube, the mucous membrane of the tympanic cavity, the cellular system of the mastoid process, the size and localization of perforation, it is possible to perform a general cavity sanitizing hearing preservation operation on the middle ear (with or without tympanoplasty), separate atticoantrotomy, tympanoplasty with revision of the tympanic cavity, attic and adympanoplasty. and myringoplasty. The question of the feasibility of a method of surgical treatment for each patient is decided individually.
Surgical intervention on the structures of the middle ear is performed under anesthesia and only in exceptional cases under local anesthesia. The larger the scope of the operation, the greater the need for general anesthesia.
Operations are performed using tools for operations on the mastoid process, a set of cutters, an operating microscope and microtools. Depending on the prevalence of the inflammatory process in the middle ear and the pneumatisation of the mastoid process, an endaural, or behind-the-ear, surgical approach is used.
The advantage of the endaural approach is a gentle treatment of tissues and a faster reparative postoperative period. The advantage of the behind-the-ear approach is the ability to more thoroughly perform the sanation of the mastoid cells and the best opportunities for mastoidoplasty.
Access paths to middle ear structures can be transmeatal and transcortical.
Hearing-saving operation
In a destructive process in the attic-antral region, widespread cholesteatoma, labyrinth complications and other cases of unfavorable course of chronic hepatitis C, which occur, in particular, repetitive 1-2 times a year, suppuration of the ear, the main method of surgical treatment is conservative-radical generalized sanitizing hearing. .
Its prototype was a radical operation on the middle ear, developed and introduced into practice in the 19th century by Zaufal, Kyustner, Bergman, L. Shtak, and subsequently modified by L.T. Levin. The purpose of the intervention is to eliminate the source of infection, prevent the development of intracranial and general otogenic complications, preserve and improve the patient's hearing, and prepare the conditions for performing the hearing-improving operation.
The operation is performed by ear access, in rare cases (with a limited destructive process) it is done through the external auditory canal.
The main stages of an all-cavitary sanitizing hearing-keeping operation:
at the first stage, the behind-the-ear incision and the separation of soft tissues are carried out, the lateral wall of the mastoid process is exposed, detachment of the posterior and partially the upper wall of the external auditory canal is carried out up to the annulus tympanicus;
in the second stage, an operation is performed on the bone; it is carried out with the help of electric cutters; a hammer and long bits with different widths of the cutting end are also used.
The following points serve as reference points for the opening of the mastoid cave: from above — the bone protrusion of the temporal line, in front — the spina suprameatum; posterior to the line bounding the triangular area of the mastoid process. A number of other anatomical structures help to navigate the surgical wound. So, above the temporal line and above the level of the upper bone wall of the external auditory canal in the middle cranial fossa is the temporal lobe of the brain covered by the dura mater. Posterior to the triangular site of the mastoid process is the sigmoid sinus. In the area of the cave entrance on the medial wall is the vertical knee of the facial nerve, and behind it is the ampulla of the horizontal semicircular canal, below which the channel of the facial nerve continues.
Boron or chisels remove the cortical bone layer, open the cells of the mastoid process and mastoid cave. The carious bone is removed to healthy bone tissue, then the posterior wall of the external auditory canal and the medial portion of the posterior bone wall (“bridge”) above the cave entrance are removed. It should be noted that the demolition of this area is associated with the risk of injury to the facial nerve and the horizontal semicircular canal located on the medial wall of the entrance to the mastoid cave. It is also important to prevent damage or dislocation of the short anvil process and its ligamentous apparatus located at the cave entrance. Therefore, this and subsequent steps of the operation are performed using an operating microscope and microtools.
They inspect the cave entrance, remove the lateral wall of the attic, revise the tympanic cavity, remove granulations, polyps, cholesteatomas, auditory of the chain of auditory ossicles, carefully release them from the granulations, retaining the functioning elements of acoustic conduction and ligamentous apparatus. Even the caries-damaged auditory ossicles in the vast majority of patients play a significant role in the conduction of sound. And, as shown by the observation of such patients after decades of surgery, the preservation in its course of the auditory ossicles (including those affected by caries) has no negative consequences.
From the skin of the posterior wall of the external auditory canal is cut out (according to A. A. Mironov) a U-shaped metotympanal flap on the feeding legs from the skin of the upper and lower walls of the external auditory canal. This flap is placed on the antrum, anvil and "spur" - a section of the posterior wall of the external auditory canal, smoothed to the level of the horizontal semicircular canal. From the remnants of the skin of the posterior wall of the external auditory canal, they cut out the lower L-shaped flap, which is placed on the lower section of the mastoid trepanation cavity.
The postoperative cavity is tamponed with turunds with antiseptics on an ointment base (levomecol, dioxycol, antibiotic with petroleum jelly) or an inflatable balloon. They put stitches on the ear wound and a bandage on the ear.
The first dressing with a change of tampons produced on the 2nd — 3rd day. In the subsequent tampons change every 2 - 3 days, periodically leaving the cavity open and irrigating it with antiseptics. After the restoration of the epidermal cover of the tympanic cavity (ie, after 3 to 4 weeks), the discharge from it completely stops. If the recovery process of the epidermis is delayed due to excessive growth of granulations, they are removed with surgical spoons and curettes and burned with a 30-40% solution of silver nitrate or tri-chloroacetic acid.
In the future, the cavity must be periodically monitored to prevent accumulation of epidermal masses in it and recurrences of suppuration from the ear.
Extended radical surgery
In case of intracranial and labyrinth complications of chronic hepatitis C patients undergo extended radical general cavity surgery. Use the ear approach with the exposure of the site of the mastoid process. With the help of burs, all cells of the mastoid process, antrum, attic are opened, the posterior wall of the auditory canal is removed, the bone bridge is smoothed, the spur is removed, if necessary, the cariously altered remains of the auditory ossicles are removed, the dura mater of the middle and posterior cranial fossa and the sigmoid sinus are removed. Further stages of the operation and management of postoperative wounds depend on the type of complication.
Atticotomy
This type of operation is shown with a limited destructive process in the vertical region and the preserved tensioned part of the eardrum. It is performed through the external auditory canal using the ear funnel or retractors. After opening the tympanic cavity with an intrameatal incision (according to Rosen), the lateral wall of the attic is removed with the aid of boron or chisels to revise this area, the auditory ossicles and their ligamentous apparatus. Ventilation of the antrum is carried out from the mesotympanum through the tympanic isthmus.
In the presence of limited (cystic) cholesteatoma or carious ossicles, all pathological contents are removed to healthy tissues and the chain of the auditory ossicles and the lateral lateral wall of the attic (closed version) are restored with various materials.
When it is impossible to carefully remove from the attic of the spreading cholesteatoma, the area of the attic is left open, separating the mesohypotympanum and antrum by autofascial graft to prevent the spread of cholesteatoma.
Atticoanthrotomy
Applied with a destructive process in the attic region and antrum with the preserved (or partially preserved) stretched part of the eardrum. The method of its implementation provides for the “expansion of atticotomy” in the posterior direction during the transmeatal approach. For this purpose, an endaural incision according to N. Heermann. After application of the retractors and the separation of the meatal flap, the posterior upper wall of the auditory canal opens. With the help of boron, the lateral wall of the attic and the aditus is removed, and then the antrum is opened. Next, resection of the posterior wall of the auditory canal is performed, which leads to the gradual expansion of the antrum (endaural surgery on L. Stacke). The surgery is completed with plastic surgery of the cavity with a meatal flap.
The transmeatal approach in the sclerosed mastoid and small antrum allows for the formation of a small mastoid cavity, which ensures its rapid epithelial distension. After opening the tympanic cavity, it is inspected and pathological tissues are removed.
A reconstructive stage of the operation is possible (tympanoplasty of the I — IV type according to Wulinteyn) using various plastic materials (autophasia of the temporalis muscle, autograss of the tragus), which are collected through the previously made access.
Separate Atticoanthrotomy with Tympanoplasty
Such an operation is indicated with limited cholesteatoma and granulations in the drum overhead and persistent sluggish HGSO with mucositis. It consists in separate removal of the lateral wall of the attic and dissection of the mastoid and antrum cells with preservation of the posterior wall of the auditory canal.
At the first stage, intrameatal access (according to Rosen) opens the tympanic cavity, makes its revision and removes pathological tissues (scars, granulations, cholesteatomas, carious auditory ossicles, thickened mucous membrane).
At the second stage, the behind-the-ear approach by transcortical boron opens the cells of the mastoid process and antrum. A prerequisite for this method is the revision and expansion of the aditus area due to its frequent block.
The operation ends various types tympanoplasty. To prevent re-blocking the aditus, a silicone film is installed for two weeks. Imposing sutures are placed on the ear wound. To ensure drainage of the tympanic cavity, the BTE wound is openly opened for two weeks. Currently, this type of operation is performed infrequently due to the complex postoperative period.
It should be remembered that chronic hepatitis C is characterized by a long course, and although sometimes the disease is accompanied by very poor symptoms, the likelihood of serious, often life-threatening complications persists. These complications often develop on the background of exacerbation of the pathological process in the ear, often in violation of the outflow of the middle ear cavity. The most dangerous of them include:
Intracranial complications: limited pachymeningitis, extra- and subdural abscess, purulent meningitis, abscess of the brain and cerebellum, sigmoid sinus thrombosis, arachnoiditis of the posterior cranial fossa; paresis or paralysis of the facial nerve; labyrinthitis.
The most reliable way to prevent these complications and preserve the patient’s hearing is to perform a sanitizing ear surgery in a timely manner.
Tympanoplasty
Surgical intervention on the ear, performed to improve hearing, is designated by the term "tympanoplasty". It is indicated for various forms of chronic suppurative otitis media, injuries, abnormal ear development, and adhesive otitis media.
The issue of tympanoplasty is solved depending on the operating findings and the state of the mucoperioste. It can be performed simultaneously with the sanitizing operation or postponed to the second stage - after normalizing the function of the auditory tube and relieving inflammatory changes in the postoperative and tympanic cavities.
Tympanoplasty involves the use of ordinary elements of the sound-conducting apparatus of the middle ear, and in the case of their partial or complete loss - the reconstruction of the transformation system using various materials. For this purpose, use:
Autogenic tissues (fascia of the temporalis muscle, cartilage with a perchondrium, a skin of the external auditory canal on the supplying pedicle); allogeneic tissues (destructive ultrathin cartilage plates, the meninges); modern bioinert materials (polyamide fabric, polyphasphasene). The chain of auditory ossicles and the eardrum are subject to recovery.
Before the operation, an audiological study is conducted, the type of hearing loss, the functional reserve of the cochlea (the difference between the thresholds of air and bone conduction on the audiogram), the ventilation and drainage functions of the auditory tube are determined. In case of a pronounced disturbance in the sound perception and functions of the auditory tube of the tympanoplastic eraser, it is ineffective. In order to predict its results, a test with a cotton swab is used - a possible increase in the severity of hearing after the operation is established. On the perforation of the tympanic membrane or in the ear canal in front of it, a cotton wool moistened with vaseline oil is placed, and find out how this changes the hearing.
For tympanoplasty to be successful, the following conditions are necessary:
The snail's functional reserve (“bone-air gap”) should be at least 20-30 dB; the functions of the auditory tube should remain at a satisfactory level, ie: - the assessment of the ventilation function (when blowing the auditory tube) should not be worse than grade II - III; - when conducting a drainage test with saccharin or dye, the time it takes for the dye to pass from the tympanic cavity to the nasopharynx should not exceed 15-20 minutes; pronounced inflammatory changes in the middle ear mucoperioste should be absent.
Contraindications to the implementation of tympanoplasty are labyrinthitis and intracranial or septicopyemic complications.
Improving hearing in tympanoplasty can be achieved in the following ways:
By enhancing the transformation of sounds; as a result of the use of sound protection (shielding of one of the labyrinth windows); with the combined use of these methods.
Various methods of tympanoplasty were systematized by X. Wuliptein, who identified five types of surgery.
Type I tympanoplasty - endaural myringoplasty (restoring the integrity of the eardrum) is performed when there is perforation in the eardrum and the normal functioning of the chain of the auditory ossicles and the auditory tube. The operation is performed through the external auditory canal using an ear funnel or retractors. Initially, de-epithelialize the edges of the perforation. After opening the tympanic cavity with an intrameatal incision (according to Rosen), all its sections (the mouth of the auditory tube, attic, aditus, retrotympanal pocket, hypothymbanum, chain of auditory ossicles and labyrinth windows) with excision (or incisions) of the hyperplastic sections of the meso-hypothympanum are excised. As a graft, a meat-implantal flap or plastic materials are used (autophasis of the temporal muscle, auricular cartilage), which are removed through additional incisions in the ear region.
Type II - performed in the presence of a defect in the head, neck or handle of the hammer. At the same time, the mobilized eardrum or nonimpymental membrane is placed on a preserved anvil.
Type III - performed in the absence of the malleus and the incus. The graft is placed directly on the stirrup head, thereby creating a “columella effect” - a bird-type sound conduction (in birds there is only one auditory bone - columella).
Type IV - shielding of the cochlea window - is carried out in the absence of all the auditory ossicles, except for the base of the stirrup. The neotympanic flap is placed on the promontory and separates the niche of the cochlea window, the hypothypomanum, and the mouth of the auditory tube. Hearing is improved by increasing the difference in pressure on the labyrinth windows.
Type V - fenestration of the horizontal semicircular canal - is performed in the absence of all the elements of the sound conductor and the fixed base of the stirrup. The surgical window is covered with a graft; at the same time, the window of the cochlea is shielded to form a small tympanic cavity, aeration of which is carried out through the lower section of the tympanic cavity.
When replacing the missing elements of the sound-conducting system, at the present time, along with autografts, various biologically inert materials are increasingly being used, such as bioceramic prostheses of the auditory ossicles or prostheses made of titanium.
Prevention of otitis media
Prevention of inflammatory diseases of the middle ear involves the elimination or weakening of the influence of those factors that contribute to the emergence of acute otitis media and its transition to chronic. Otitis prophylaxis should be started from early childhood.
In infants, the level of natural resistance is directly dependent on the method of feeding. With breast milk, the baby receives substances that provide non-specific humoral protection, for example, lysozyme, immunoglobulins, which is very important for the adaptation of the child to environmental conditions. Therefore, an important preventive measure catarrhal diseases and otitis media is feeding the baby with breast milk.
If, until recently, the incidence of otitis media in young children was mainly due to children infectious diseases, today, thanks to mass specific prophylaxis, it has been possible to reduce the incidence of such infections as measles and scarlet fever.
A number of other factors also affect the incidence of otitis media in children and adults:
High prevalence of respiratory viral infections, reducing the mucociliary activity of the respiratory epithelium (including the epithelium of the auditory tube) and suppressing the local immune defense; . widespread, often unsystematic and unreasonable use of antibiotics, which leads to resistant strains pathogens and at the same time violates the body's natural defenses. . sensitization of the body and the perversion of the mechanisms of local and general immune protection, developed by eating foods containing preservatives and / or various synthetic additives, and in children arising from artificial feeding. . decrease in the general nonspecific resistance of the organism due to hypodynamia, limited exposure to the open air and the sun, insufficient intake of vitamin-rich foods.
Elimination of the adverse effects of these factors will reduce the frequency of inflammatory diseases of the middle ear.
Chronic foci of infection in the nose and throat play an important role in the development of acute otitis media and in its transition to chronic. Timely rehabilitation of such foci of infection and restoration of normal nasal breathing are necessary components in the complex of measures to prevent otitis media.
The best prevention of chronic suppurative otitis media is the correct treatment of a patient with acute otitis media. An important component of such treatment is timely (if indicated) performed paracentesis, as well as adequate antibiotic therapy, prescribed taking into account the characteristics of the pathogen and its sensitivity to antibiotics.
It should be borne in mind that long-lasting many years of remission during chronic otitis often create the appearance of well-being for both the patient and the doctor. However, even with a calm clinical picture of a chronic purulent otitis media, a patient can form a cholesteatoma or an extensive carious process in the cavities of the middle ear, which can lead not only to increasing hearing loss, but also to the development of serious, often life-threatening, complications. Therefore, the sooner the ear is sanitized, the greater the chances of preserving and improving hearing.
Popular
- Why seals may appear
- Blood disorders in children
- What can not drink a pill
- Blood disorders in children
- Blood disorders in children
- Bones: structure, composition, types of bones, types of compounds and their characteristics
- How many live with lung cancer
- Influenza in children: how to treat, what can and cannot be done to parents, what medicines will help?
- "They are people too ..." - you say
- What helps "Prednisolone"